So let’s not beat around the bush here: a significant number of people – not only in America but around the world – have tried or habitually done marijuana sometime in their lives, legally or illegally, for medicinal purposes or as a recreational drug. That being said, you would think that people would be clamoring to educate themselves and others on the risks and benefits associated with its use. I don’t know about the users, but there are plenty of scientists out there aiming to do just that, particularly in regard to the relation of cannabis and neuropsychiatric disorders. There are certainly therapeutic applications, but more research is needed to avoid some unwanted side effects.
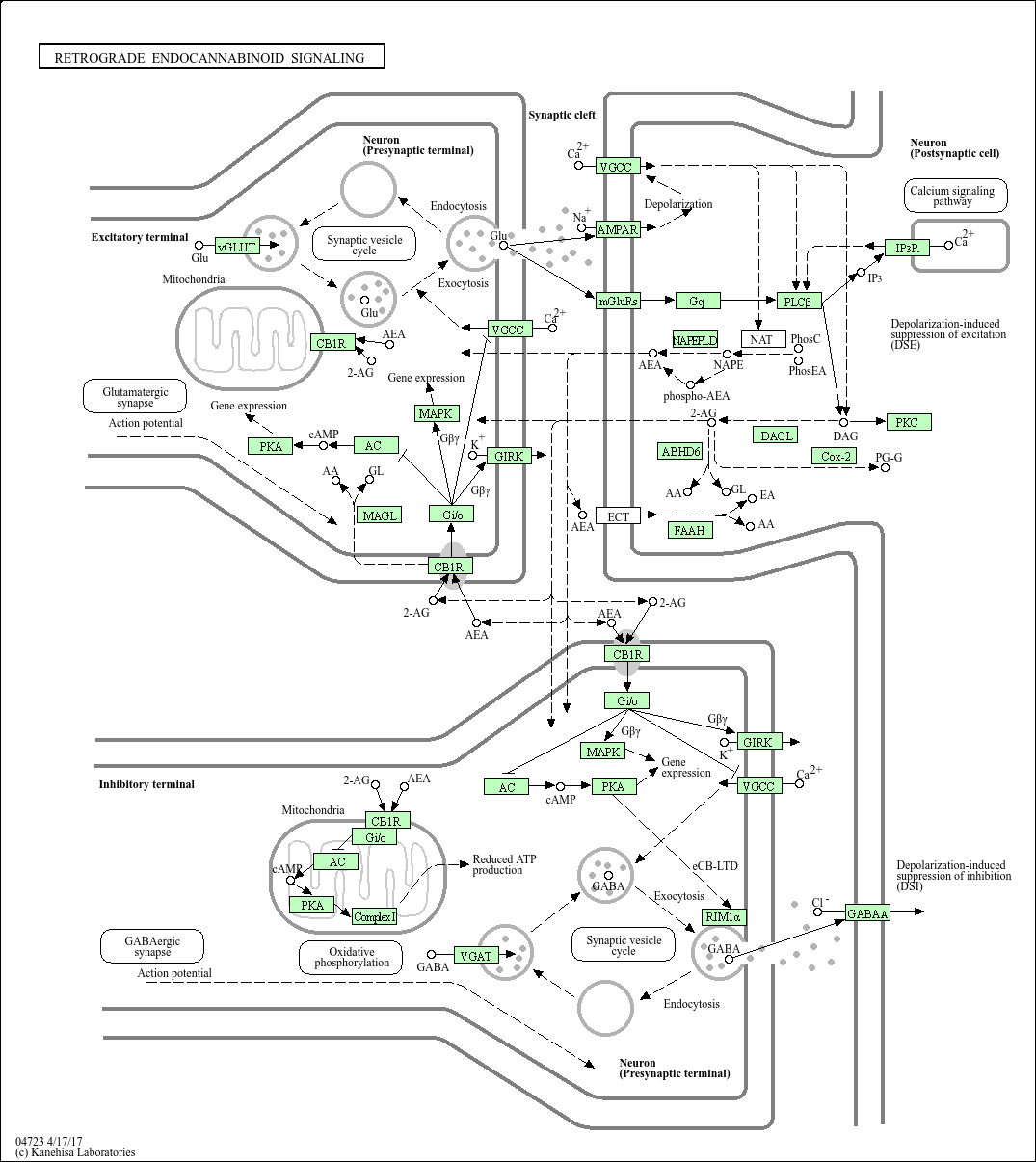
Cannabis (marijuana) has two main active ingredients: tetrahydrocannabinol (THC) and cannabidiol (CBD). These two compounds interact with the brain via the endocannabinoid (eCB) system, activating ligand-binding cannabinoid receptors (CB1 and CB2). It’s through these two receptors that most of the action happens, whether ultimately beneficial or detrimental. THC is the addictive, psychoactive, and “munchies”-inducing contributor to cannabis that has also been suggested to cause anxiety. CBD is attributed with many therapeutic effects, which includes treatment of spasticity in multiple sclerosis patients, inhibiting cancer growth (most notably in breast cancer), and being an antipsychotic for treating schizophrenia. It interacts with the eCB system as an antagonist to the two receptors in low doses, and increases CB1 expression in high doses.
The eCB system has been shown to be extremely influential in neuropsychiatric disorders such as anxiety, depression, and schizophrenia. Its effects, however, are both positive and negative. For example, the CB1 receptor is involved with inducing anxiety when it’s expressed on one type of neuron (glutamate) and relieves anxiety when expressed on another (GABA). You can see why things can get a little messy.
Here’s an overview of the results linking the eCB system with these disorders:
- CB1 expressed with GABA relieves anxiety
- CB1 expression likely helps avoid depression (deletion enhances depression)
- CB2 overexpression relieves anxiety
- CB2 likely decreases vulnerability toward depression
- Presence of CB2 seemingly reduces the risk of developing schizophrenia
- CB1 expressed with glutamate induces anxiety
- Prolonged activation of receptors increases the risk of developing schizophrenia
The negative aspects seem to tap into the subtle complexities of the eCB system and neurological signaling in general – pathways are often very convoluted and activation or inhibition often have multiple different effects, influencing many different pathways. One particular pattern I’ve noticed is that dose and frequency of use play a significant part in the ultimate effects due to receptor activation. For example, low doses of cannabis seem to give a calming, anxiety-relieving effect, but high doses actually lead to anxiety, paranoia, and psychosis. Also, it seems that activation of the CB2 receptor is necessary to decrease one’s risk of developing schizophrenia, whereas prolonged activation of the eCB system increases this risk. Most confusing of all, testing for these neuropsychiatric disorders with eCB agonists and antagonists with the same receptor expression gave different results across groups. All of this says one thing to me: we have quite a long way to go to characterize exactly what’s going on with the eCB system and these disorders.
There seems to be a strong basis of hope for cannabis-related drugs in the treatment of many different illnesses. Cannabidiol itself has fantastic applications for the treatment of multiple sclerosis and cancer, among many other things, and has been shown to positively affect people with neuropsychiatric disorders, relieving anxiety, acting as an antidepressant, and protecting against psychotic reactions and symptoms. However, cannabis does not look like the answer, due to its adverse effects from THC (anxiety-inducing, addictiveness, etc). There is great potential in the study of cannabis and cannabinoid substances in medicine, but cannabidiol seems to have a lot more promise than cannabis. In either case, before cannabinoids are highly implemented in medicine there should be greater definition of the mechanisms through which they work, so as to define safe dosage and ensure that the pros really outweigh the cons. Like that withdrawal party…