Alzheimer’s is the only disease among the top 10 causes of death in America that cannot be prevented, cured or even slowed. Current treatments have varying effectiveness for different people, of course, however, in general, the average patient cannot find relief or delay in the progression of the disease. With 1 in 3 seniors dying from Alzheimer’s or another dementia and AD (Alzheimer’s Disease) being the 6th leading cause of death in the United States, it makes sense that this is a very active area of research. A new promising target for future AD treatment targeting is the protein Tau.
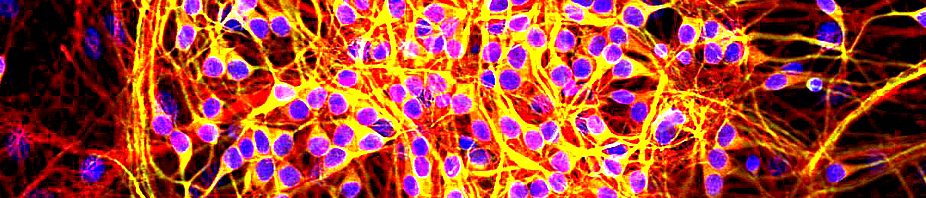
Before we get into Tau and its relevance, we should set up how AD changes the brain. The main characteristic of AD is dementia, memory loss. Dementia is caused by blockage of neuronal signaling and neuronal death, especially in the Hippocampus, which is the area of the brain that memory is associated with. There are two major players, Beta Amyloid and Tau. Both are proteins with necessary functions, but incorrect cutting or modifying leads to negative consequences. Beta Amyloid Plaque is the classic attribute of AD. What happens is Amyloid is cut incorrectly and begins to clump together. These clumps occur between cells and continue to grow over time. The plaque can cause Dementia in two ways, it can block neuronal communication which wouldn’t allow memory formation or recall, and it can also cause an inflammatory response leading to cell death, like when you puff up from a bug bite. Most treatment has been focused on Beta Amyloid Plaques because of how visible they are in the brain in AD patients, so naturally, they would be seen as a target for treatment.

Amyloid Plaques certainly do contribute to AD, however, recent research has shown that Tau levels and clumping together may better mirror AD development and symptoms. This is exciting news since current treatments aren’t very effective and a new drug target may be exactly what we need. Tau’s regular functions are much more important to understand for its role in AD. Tau helps stabilize something in the cell called the cytoskeleton. The cytoskeleton works much like our own, holding the cell in its form, but it also serves as the highway system of the cell to move nutrients, proteins, and organelles around. What happens in AD is that Tau is changed incorrectly so that it can’t stabilize the cytoskeleton. This leads to a dysfunctional skeleton and left-over Tau. The breakdown of the highway system leads to less efficient communication between cells and ultimately cell death, both contribute to dementia. Then, much like the plaques, Tau aggregates (groups together) at first in small clumps, but then eventually large groups that no longer dissolve in water (insoluble), same as plaques. These groupings are within the cell at first, however, they eventually burst out of the cell creating Neurofibrillary Tangles. This causes cell death and then the tangles continue to spread with the progression of the disease.

Tau is an exciting prospect for AD treatment, not only because any new treatment could help, but because we’re finding out that it may be the major agent causing AD, not the classically understood Beta Amyloid Plaques. This discovery follows the development of imaging techniques to the point where a PET scan can observe the levels of Tau, Beta Amyloid, and rate of metabolism in cells (energy burning). These new imaging techniques have allowed us to see that in patients with AD, increased Tau levels associate more closely with the progression of the disease and cell death than Amyloid. It has even been presented that Tau might be one of the first players in AD, well before Amyloid, possibly even causing Beta Amyloid Plaque formation. In light of the ineffectiveness of AD treatment, this new target offers hope of managing and maybe even preventing Alzheimer’s disease. Future treatment will focus on stopping the wrong modification of Tau and not allowing aggregation, targeting pathological tau proteins for degradation along with dissolving aggregations of Tau. Hopefully, these new avenues bring hope to those with AD, however, this is a very recent discovery and drug development and refinement will take some time.
A New Focus for Alzheimer’s Disease Treatment: Tau Protein