In 1970, cannabis was placed as a schedule I drug under the Controlled Substance Act (CSA). Schedule I substances are defined by the DEA as drugs without an accepted medical use, high abuse potential, and potential of severe psychological or physical dependence. Since cannabis was denoted a schedule I in 1970, there has been controversy on whether cannabis should be a schedule II. Schedule II substances have a high abuse potential and a potential of psychological or physical dependence (DEA, 2015).
The main differences between Schedule I and II are the severity of the potential danger and the potential medical use of the substance. In order to do clinical research for potential medical uses of cannabis, the researcher must have a DEA license and approval from the FDA. As a schedule I drug, cannabis is difficult for researchers to obtain. To obtain the substance, the researcher has to go through the National Institute on Drug Abuse (NIDA). These steps a researcher has to go through to obtain and research a schedule I drug tend to be problematic and limiting the amount of studies conducted within the United States. Therefore, most studies have been done on tetrahydrocannabinol (THC), a component of cannabis, and cannabinoids.
There are more than 60 compounds in cannabis. THC is the most studied of the components and is psychoactive. It can be ingested or inhaled and is commonly thought of as the “high” component of cannabis. THC works by binding to cannabinoid receptors, the most prominent receptor found within the body. Another compound is cannabidiol (CBD) which is non-psychoactive and is thought to contain the medicinal effects of cannabis. THC and CBD work synergistically enhancing their effects, known as the Entourage Effect. This explains that both, THC and CBD, need to be present for medical benefits, however, THC can be at a much lower concentration for medical marijuana (cannabis).

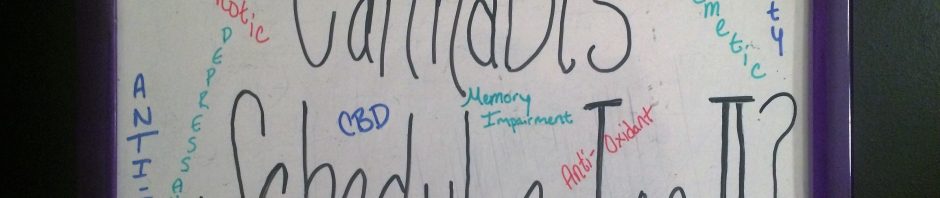
Cannabis has several studies from other countries that support medical use. The American Academy of Neurology supports the use of cannabinoids for multiple sclerosis (MS). Evidence supports improvements in spasticity and reduction of central pain in MS. The US National Cancer Institute suggests evidence of cannabis use for cancer-related pain and vomiting (antiemetic). Other possible areas of treatment are with HIV neuropathy, depression, and neurodegenerative disorders. There are presumed disadvantages of cannabis. These include anxiety, dysphoria, euphoria, hallucinations, paranoia, acute memory impairment and reduced cognitive function. Smoking cannabis is thought to have an effect on the increase in airway diseases, risk of schizophrenia, and oropharyngeal cancers.
In the US, there has been 28 states and DC to legalize medical marijuana, including Minnesota. Other states have legalized the use of the non-psychoactive extract called CBD. There are 7 states and the District of Columbia which have legalized the recreational use of marijuana. Nearly half of US citizens have used cannabis once in their life. A common misconception is lowering cannabis to a schedule II drug will increase the likelihood of it being used recreationally, but I believe it should be lowered for the use of research on further potential medical uses and long-term effects of cannabis. The United States has moved forward with medical uses for cannabis, but it continues to be a schedule one. Researchers have difficulty accessing it, yet it has been legalized in many states. Questions about the long-term effects are prevalent in the US, but we must rely on other countries to continue the research. Many people here in the US have access to cannabis for health benefits, but researchers struggle to gain access to it to understand the mechanism, long-term use effect, or how else it may be used.
Should Cannabis Be Schedule I?