You’re Not YOU
Picture this: You are 29 years old, in shape, happily married, thinking of children, an avid baker, and enjoying playing the piano in the evenings as you sip your daily glass of red wine. Could life get any better?
Suddenly, one day you start to notice unusual, yet slight tremors in your fingers. You don’t think anything of it. But then those tremors get larger, more pronounced, enough to disrupt your usual evening piano recital and eject the glass of red wine from your hand. Welcome to the beginning of one of the most relentless and soul-robbing diseases today: Amyotrophic Lateral Sclerosis (ALS) or Lou Gehrig’s Disease.
Meet Kate, a classical pianist who is diagnosed with ALS and the star of the movie shown below, “You’re Not You.” Throughout the span of a few years, Kate experiences the progressive weakening and atrophy of her voluntary muscles that rob her of the life she loved to live. If you would like to experience the life of an ALS victim through the eyes of Hollywood drama, spend your Saturday afternoon sobbing and watching “You’re Not You.”
What is ALS?
ALS is a fatal motor neuron disease that is characterized by the weakening and atrophy of both upper and lower motor neurons. Normally upper motor neurons in the brain function to send signals to facial and cranial muscles, as well as to lower motor neurons located in the brain stem and spinal cord. The lower motor neurons then send signals out to respective muscles and cause contraction of those muscles to aid in our voluntary movements, such as talking, swallowing, breathing, and walking.
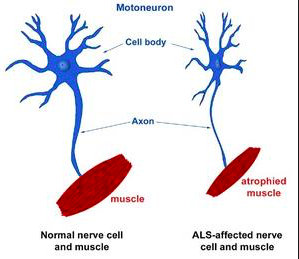 Figure 1. Depiction of a healthy motor neuron and an atrophied motor neuron seen in ALS.
Figure 1. Depiction of a healthy motor neuron and an atrophied motor neuron seen in ALS.
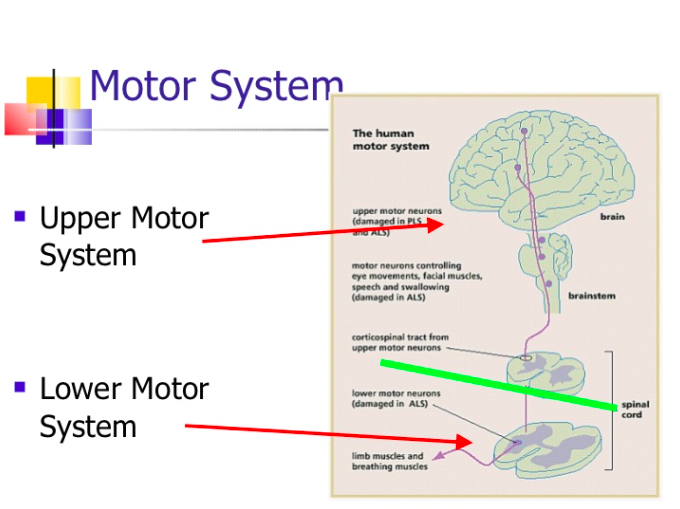 Figure 2. General locations of the upper and lower motor systems in the body.
Figure 2. General locations of the upper and lower motor systems in the body.
Trapped
Although all voluntary muscles are affected by ALS, the cognitive state of victims usually remains in tact. Some would argue that this makes ALS even more torturous for its victims to suffer through. This relentless disease almost always results in respiratory failure and death within a few short years (3-5 years) after initial diagnosis.
The ALS Brain
There are four interconnected pathways identified in the vicious cycle and progression of ALS that specifically affect both the upper and lower motor neurons of ALS victims. Researchers are currently unsure which part(s) of these four pathways is responsible for initiating this vicious cycle. These pathway outcomes ultimately lead to the associated symptoms of ALS:
1. SOD1 and Oxidative Stress
Many ALS cases involve mutations (genetically inherited or sporadic mutation) of the gene encoding the superoxide dismutase enzyme (SOD1). SOD1 functions as a cytosolic antioxidant enzyme, defending against reactive oxygen species (ROS) formed in cells during normal cellular metabolism. When the SOD1 gene is mutated, SOD1 enzyme is defective, which leads to a buildup of ROS in the brain and ultimately oxidative stress. The oxidative stress overpowers cellular organelles and leads to organelle dysfunction. The cellular organelle dysfunction leads to defective cellular metabolism and protein production and a prolonging of cellular oxidative stress.
2. Protein Folding
An increase in oxidative stress leads to the aggregation of misfolded proteins, which overpowers the body’s natural autophagy system (responsible for cleaning up misfolded proteins and defective organelles) and renders it dysfunctional. This amplifies the buildup of misfolded proteins in cells.
3. RNA Dysfunction
When under stress, the cell halts translation via the formation of stress granules in the cytoplasm: globules of non-translating mRNA, ribosomal subunits, and translation initiation factors (think of wads of gum). During prolonged oxidative stress, however, permanent stress granules form that cause important molecules in RNA processing and protein production (FUS and TDP43) to aggregate and render them nonfunctional. The stress granules are similar to wads of gum that stick to anything they touch, including FUS and TDP43. The failure of FUS and TDP43 to carry out RNA processing leads to dysfunctional RNA processing and protein production. This further amplifies cellular oxidative stress.
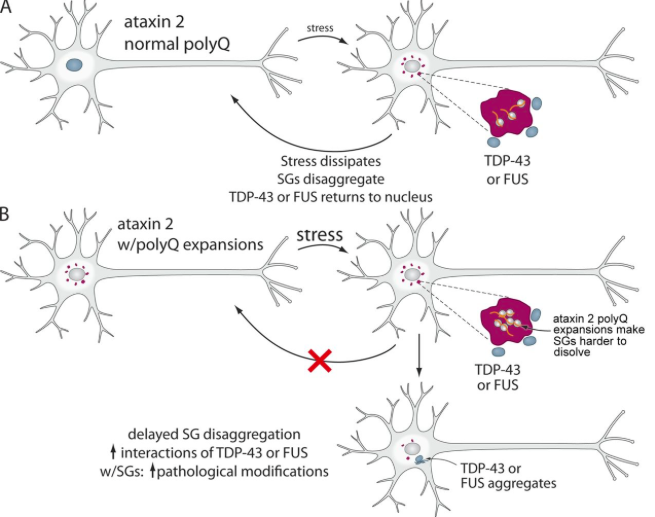 Figure 3. The formation of permanent stress granules in the cytoplasm and consequent aggregation of TDP43 and FUS.
Figure 3. The formation of permanent stress granules in the cytoplasm and consequent aggregation of TDP43 and FUS.
4. Metal Ion Homeostasis
An altered metabolism and increase in cellular levels of iron and copper lead to an increase in cellular ROS. This increases the oxidative stress in the body, amplifying the dysfunctional RNA processing mentioned before, and ultimately protein degradation within the cells.
The Future of ALS
Currently, there is no cure for this horrible, life-altering disease. However, there are multiple therapeutic options (physical therapy, occupational therapy, rehabilitation) to help ALS victims. There are also standard pharmaceuticals administered for pain relief and to aid in prolonging life, such as edaravone. Riluzole is a drug that has been shown to prolong the life of an ALS victim 2-3 months without treating symptoms of the disease.
The future of ALS lies in the hands of scientific researchers and the study of brains of ALS victims to develop a better understanding of the disease’s actions. Further pathways of the disease need to be identified in order to find potential therapeutic targets that may lead to the cure of ALS or a greater prolonging of life of ALS victims.
If you would like to learn more about the physiology of ALS, please visit:
http://www.sciencedirect.com/science/article/pii/S0304394016302877?via%3Dihub
Images From:
https://kin450-neurophysiology.wikispaces.com/ALS+II
https://www.slideshare.net/santhurao/physiology-859392
http://jcb.rupress.org/content/201/3/361
