Linking Alzheimer’s Disease and Type II Diabetes
The Link
When picturing an individual suffering from Alzheimer’s disease (AD) and one suffering from Type II Diabetes (T2D), these pictures look greatly different. However, zooming in past the physical symptoms and appearances, we can look closely at the specific ways these disorders work. Tied together by the mechanisms of neuroinflammation, insulin resistance, and ganglioside function, AD and T2D are more similar than we might imagine.
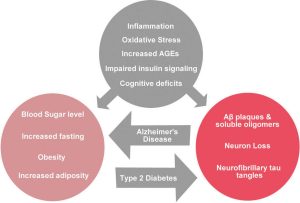
Image 1: The biological connections in grey can be studied between AD and T2D and represent the two-way street these disorders pave in our brains.
What is Insulin?
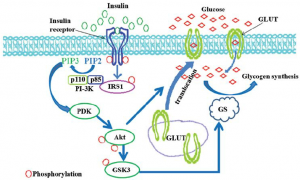
Insulin is a hormone generally made in the pancreas that helps our body take in glucose, which is processed and used for energy and stored in our cells for future use. In diabetes, this process does not function. In type II diabetics, insulin is produced but not able to complete the signaling pathway to intake glucose.
The Pathway:
Insulin leads to the uptake of glucose through the pathway represented in the above image. Insulin binds to the transmembrane insulin receptor (IR). This activates the IRS1, leading to a phosphorylation cascade ending with the translocation of GLUT receptors to lipid rafts (compartmentalized sections) in the membrane.
Understanding Alzheimer’s:
Alzheimer’s disease is characterized by the buildup of amyloid plaques and neurofibrillary tangles in the brain. The pathway to these malformations is complex, but has many connections to neuroinflammation and insulin resistance.
Connecting the Pieces
The pathways of AD and T2D connect through insulin resistance and neuroinflammation. The two figures below detail the complex mechanical connections between the diseases. More specific information on these topics can be found at source links 1 and 2 below.

Image 3: Insulin resistance affects the production of glucose peripherally. This dysfunction in the CNS contributes to the formation of amyloid beta plaques and neurofibrillary tangles in the brain.
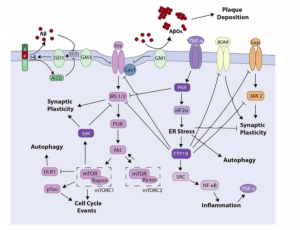
Image 4: This pathway shows that many factors (ex: PKR, S6K, PTP18, GM3) directly inhibit the processing of insulin. The buildup of GM3 molecules physically disassociates the IR from its connection with IRS 1/2, causing reception to be halted. The GD3 molecules that are made from GM3 perpetuate the buildup of Amyloid Beta plaques, showcasing the connection to AD.
So what?
Using the connections in mechanism between T2D and AD can inform future treatment options and research in both conditions. Seeing the parallel nature in pathophysiology between the conditions, it isn’t surprising how often the two disorders overlap. The knowledge gained from a dual-perspective view at both AD and T2D can influence further research in not only these conditions, but also other neurodegenerative conditions involving neuroinflammation due to the buildup of malformed molecules in the brain. This research has the potential to impact a large community of individuals and family members who are affected by neurodegenerative diseases or Type II Diabetes.
Sources for further research
- https://www.researchgate.net/figure/Schematic-diagram-of-the-insulin-signaling-pathway-Binding-of-insulin-to-the-a-subunit_fig2_232231667
- http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1980-57642017000200105
- https://www.abcam.com/pathways/overview-of-insulin-signaling-pathways
- http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1980-57642017000200105
- https://www.google.com/search?biw=1241&bih=715&tbm=isch&sa=1&ei=WRa8W6OxPO-l_QbNw6-ICA&q=alzheimers+and+diabetes&oq=alzheimers+and+diabetes&gs_l=img.3..0i10i24.15202.17476..17593…1.0..0.297.2054.4j5j4……1….1..gws-wiz-img…….0j0i10.cMHLL_jyY7Y#imgrc=67SBnaVcq0xlOM: