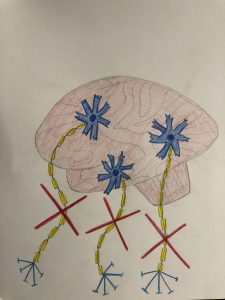
ALS, or amyotrophic lateral sclerosis, is a neurodegenerative disease that affects neurons in the brain and spinal cord. This disease is characterized by muscle atrophy, as the neurons that signal and control the muscles are targeted for degeneration. This causes sclerosis, which is scarring or hardening of tissue. The disease is typically diagnosed between ages 40 and 70. There are two types of ALS: sporadic and familial.
-
-
-
- Sporadic: most common form of ALS; can affect anyone
- Familial: accounts for 5-10% of all cases of ALS; inherited disease
-
-
Symptoms of ALS get worse over time and there is currently no cure for the disease. Most people diagnosed with ALS die about 3-5 years after diagnosis, often from respiratory failure. Common symptoms of ALS include:
-
-
-
- Fasciculations, or muscle twitches
- Muscle cramps
- Tight/stiff muscles, or spasticity
- Muscle weakness
- Slurred speech
- Difficulty chewing and swallowing
-
-
As the disease progresses, individuals may experience difficulty moving, speaking or forming words, and breathing, as well as difficulty with some mental processes. As there is no cure for ALS currently, it is treated mostly to control and slow down symptoms. Treatment is mostly provided by supportive care to keep individuals as mobile and comfortable as possible. Medication, physical therapy, speech therapy, nutritional support, and breathing support are some of the specific treatments available. Despite all of these treatments, the disease can only be slowed down so much.

Due to the fast progression of the disease, much of the focus of ALS is on end-of-life care. There is a large controversy about how to handle this disease toward the end of someone’s life, what treatments should be done, and who should be able to make final decisions during that time. Some of the biggest questions surrounding this topic include:
-
-
-
- Hospice
- Physician-assisted suicide
- Decisions at end-of-life
-
-
The discussion surrounding hospice is whether or not it is right to stop curing/treating the illness, as well as who decides whether or not the individual should enter hospice care. Hospice is meant for when the illness can no longer be cured and the individual has 6 months or less to live. Hospice is meant to keep the patient comfortable and only provide relief for the symptoms. It is difficult for many individuals to accept that there is no further treatment, that they have less than 6 months to live, and that they will have to spend the rest of their life without any control until they die. This leads to the controversy with physician-assisted suicide. Many people believe that a person diagnosed with ALS should be able to choose this option toward the end of their life in order to stop them uncontrollably watching themselves losing motor control and slowly dying. The main reason for supporting this decision is to avoid pain and suffering, leave the world with dignity and peace, and reduce health care costs. However, others believe that there should be no reason for anyone to choose to die and that it is selfish to choose this option when they have a family or other people in their lives. It is also an argument that people near death should not be responsible for making the decision to take their own life. Many people see physician-assisted suicide as breaking the oath a doctor takes to preserve lives and increasing the value of human life. Finally, the question about who is expected to make the decisions toward an individual’s end of life is often controversial. It is based on a thin line between whether or not the diagnosed individual is able to make their own decision or if the family must make final decisions for them.

All of these issues create difficult conversations when dealing with ALS and causes struggles when deciding treatment plans for individuals after diagnosis. In order to provide the best care for patients, it is important to keep the patient’s wants and needs as a priority and make decisions based off of what is best for the patient and the remainder of their life.