What should insulin be doing?
You’ve probably heard of insulin before but role does it actual play in our bodies? When functioning normally, insulin helps regulate our blood sugar levels by breaking down carbohydrates into different pieces. One of those pieces is glucose which is our bodies main form of energy. Once this glucose is in our bloodstream, the pancreas starts producing insulin which lets glucose into our body’s cells to give them energy. Your body can also store this insulin in muscles, fat cells and liver to be used later if needed.
What does it do in Alzheimer’s Disease (AD)?
Insulin has also been found to protective of the neurons in our brain making it important for cognition, something we know is implicated in AD! The brain is an insulin sensitive organ and insulin has been found to promote memory functioning within it. So, if there is an issue with insulin, there can be an issue with memory and cognition.
What does it do in Type 2 Diabetes (T2D)?
Insulin is most usually talked about in the context of Type 2 Diabetes. With this condition, glucose levels keep rising because the insulin is not moving the glucose into our cells effectively. It’s not that those with Type 2 Diabetes don’t have insulin, they just usually are not using it effectively or don’t produce enough, insulin resistance and insulin deficiency, respectively.
So… how are they connected??
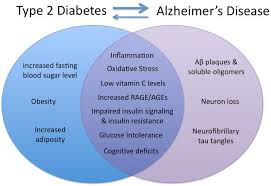
There appears to be a connection between Type 2 Diabetes and Alzheimer’s as patients who develop one are more likely to develop the other. This means if you get Alzheimer’s, your chances of getting T2D are higher than the rest of the population.
Maybe brain inflammation?

When researchers look at the brains of those with Alzheimer’s they find evidence of issues with insulin signaling. A proposed link between the two is the inflammation that occurs when there is a fat accumulation seen in the body in T2D or the sustained inflammation seen in Alzheimer’s brains. It suggested that this inflammation could be due to a specific inflammatory cytokine called TNF-a that induces insulin resistance.
Maybe gangliosides promote insulin resistance?
AD is characterized by a plaque build-up on the neuronal level referred to as amyloid beta plaques. When these plaques start to build up, a number of other cells cannot perform their usual functions or jobs, dysregulating a lot of other pathways. A ganglioside called GM3 is important in cell metabolism and it’s possible that when these plaques build up, the GM3 cannot do its job and so the downstream signal is blocked leading to insulin resistance.
Could be mTOR deregulation? The evaluation of mTOR can lead to insulin resistance.
Could be issues with PTP1B? Elevated PTP1B is found in T2D and could regulate neuronal inflammation.
What now?
It’s clear we won’t have all the information about the pathology of either AD or T2D nor do we understand fully the connections between the two. In this short post, I have only scratched the surface of the depth of these potential connections but it’s difficult to determine what causes what. Does inflammation cause a build of plaques, or vice versa? Which comes first? Does the mTOR pathway affect the amyloid beta plaques? We know a number of these things are connected but we don’t know where to start in the pathway. More research on these factors could break open the treatment options for AD and T2D- we just need to figure out where to begin.
https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-treatment/art-20044084