While diet fads come and go, in the end physicians typically boil there advice down to a simple statement; burn more calories than you eat and you’ll lose weight. Unfortunately, this oversimplification of a very precariously balanced regulatory system in the human body leads to a lot of shame for people who simply can’t keep the weight off. This isn’t a problem facing a few Americans, this is a national epidemic. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), 1 in 3 adults are overweight, and 1 in 3 adults are considered obese meaning that a combined 2 out of 3 adults are above their normal weight based on the 2013-2014 survey. This epidemic is far too large to be placing personal blame on every individual. This is not to say that personal choice does not play a role; each and every person must make decisions to eat as healthy as possible within their means as well as dedicating time to exercising. That being said, sometimes its not enough.
What’s the brain got to do with it?
Unlike many common conceptions, obesity is not simply because people are being  lazy and eating food that is bad for them. While factors such as eating habits, exercise, and screen time all contribute to a person’s weight, so do medications, chronic illnesses, socioeconomic status, and access to healthy foods. Genetic predisposition has also recently been shown to play a major role in a person’s weight. What many people don’t know is that chemical changes in the brain are partially, if not largely, responsible for obesity and can be induced by outside factors.
lazy and eating food that is bad for them. While factors such as eating habits, exercise, and screen time all contribute to a person’s weight, so do medications, chronic illnesses, socioeconomic status, and access to healthy foods. Genetic predisposition has also recently been shown to play a major role in a person’s weight. What many people don’t know is that chemical changes in the brain are partially, if not largely, responsible for obesity and can be induced by outside factors.
ER Stress May be Limiting Diet Success
Leptin is one of the main hormones in your body responsible for maintaining balance when you eat.
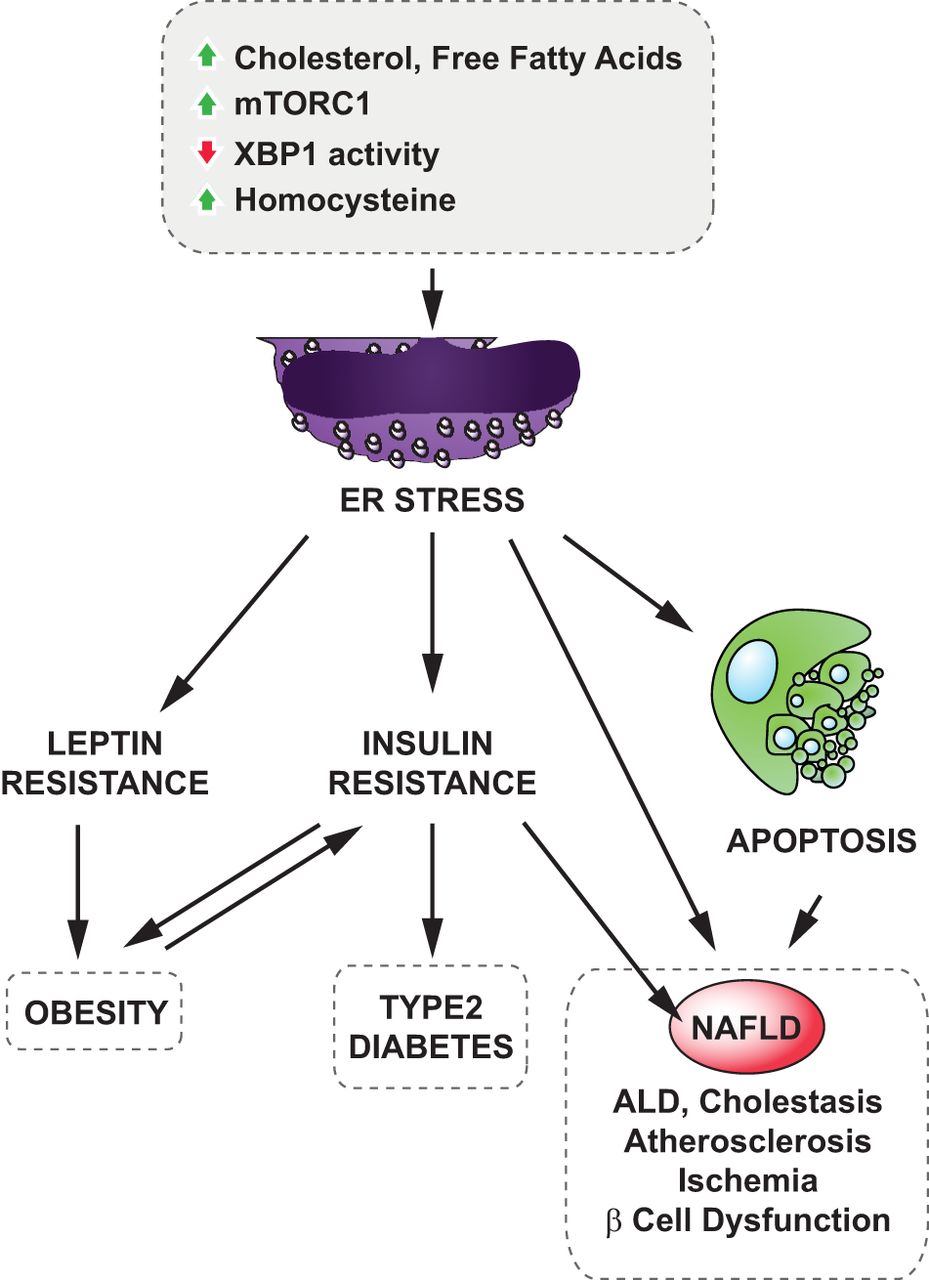
It suppresses appetite and also regulates how much energy your body spends. Working alongside leptin is insulin, which allows your body to use the energy from the food that you eat. When the body becomes resistant to leptin and insulin, energy usage and eating habits get out of whack. New research suggests that endoplasmic reticulum (ER) stress induced by biochemical changes could be responsible. Check out the figure to the right for the data on this. As is shown, when a Western Diet (i.e. high in fat) increases cholesterol and free fatty acids, changes to stress states can result in increased homocysteine and a variety of other changes. This put the ER under stress, which is particularly bad because cells need a functioning ER to maintain proper proteins.
So, what’s the link to leptin and insulin? Well, once the ER is under stress, it sets off a cascade known as the unfolded protein response. In this response shown in the figure, cellular metabolism is altered, and inflammatory actions are dramatically increased.
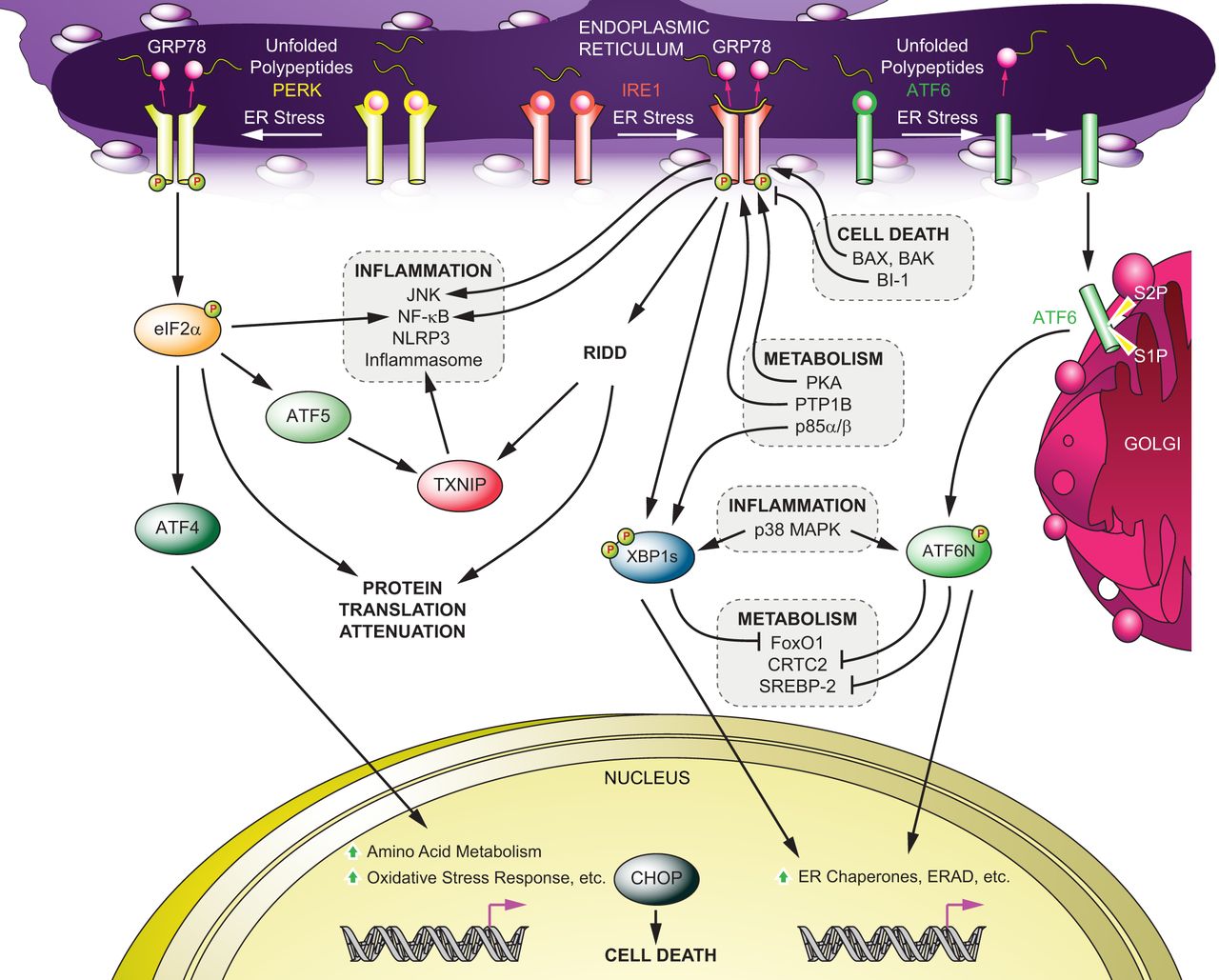
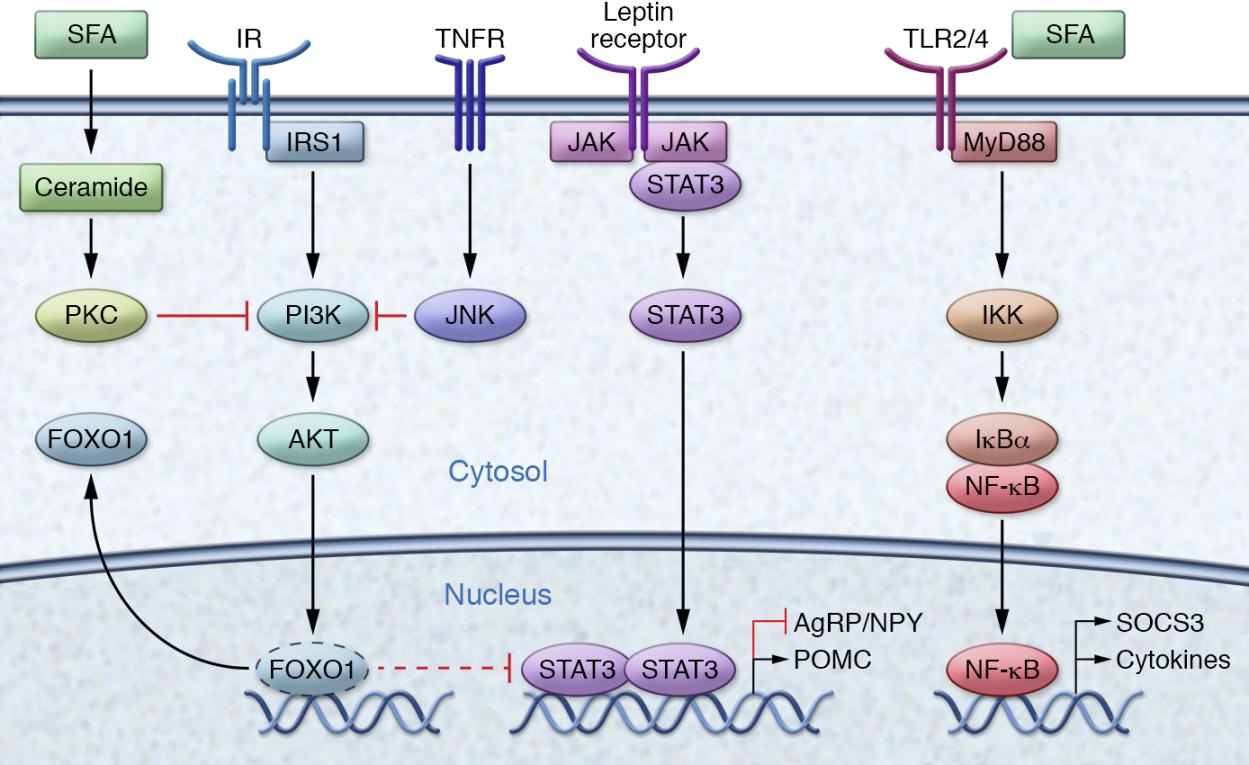
This inflammation, specifically NF-κB proteins, alters DNA transcription and results in the transcription of SOCS, or the suppressor of cytokine signaling. This inhibits specific JAK-STAT signaling, which is the mechanism that the leptin hormone works through. This hormone is tied intrinsically to the insulin pathway, which makes the situation worse. Furthermore, this is just one small problem going on in the cell. Inflammation and other pathways and receptors are being targeted as well, resulting in massive changes to the microenvironment in the hypothalamus, the region of the brain responsible for regulating food intake. These can be seen in the figure below, with the full paper here.
What’s the takeaway?
Obesity is a massively complicated issue stemming from a variety of personal, biologic, and societal issues. It is causing a huge health burden to the world and especially the US. While personal responsibility in making good food and exercise choices is important, exclusive blame can’t be laid at the backs of the patients. Fast food, whether it is in a drive thru line or a box at the grocery store is changing our diets and not for the better. Understanding the complex web of factors that contribute to this crisis is a good first step. Most importantly, changing our narrative about obesity and empowering the medical community to seek out new ideas and solutions is the only way to eradicate this epidemic.
