We all recall the impossible question of “What comes first, the chicken or the egg?” This questions causes those to spiral in the possibility of both scenarios where the egg to needs to bring the chicken and the chicken needs to lay the egg. There is no cohesive answer.
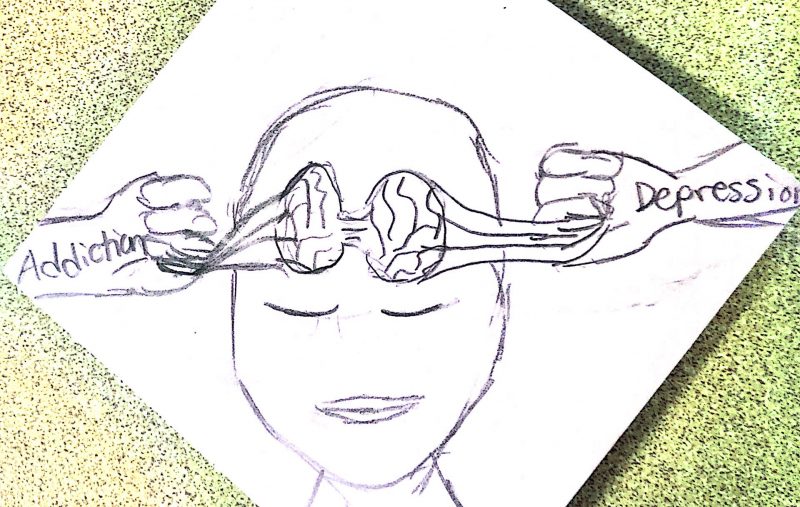
Another form of this question currently is a major topic of interest in research. Does mental illness bring about addictive tendencies or vice versa, addictive tendencies bring about bouts of depression and anxiety?
One study found that roughly 37% of alcoholics and 53% of substance abusers have at least one mental illness diagnosis or meet the diagnostic criterion for a mental illness. Though seems like a straight shot answer, keep in mind that it was also found that 29% of those diagnosed with at least one mental illness also abused alcohol or other substances. Even extending into adolescent study, 60% of individuals in a substance abuse rehabilitation facility either have a diagnosis or meet the diagnostic criterion for a mental illness.
The most common mental illnesses to be seem in a comorbid relationship with substance abuse are those that appear to have a dysregulation in dopamine signaling and/or excitatory and inhibitory neurotransmission, physiologically represented by depressive episodes. These mental illnesses include Bipolar Disorder, Depression, ADHD, and Schizophrenia. If any of the previously listed disorders significantly impact the quality of the life of the individual, they are more likely to fall into substance abuse to satisfy the lack of serotonin and get a sense of “euphoria.” 1 in 4 diagnosed with serious mental illness abuse some substance.

Figure 1: Rate of Dual Diagnosis between substance abuse and serious mental illness.
As you can see, this poses a major concern about going about treatment. If someone has a serious mental illness, psychiatrists may begin to lean to stronger medications, such as Xanax. However, unless it is openly addressed about addictive tendencies of the individual, they may accidentally begin a downward spiral of prescription medication addiction. Addictive tendencies can have a hereditary nature, so having open communication with patient and practitioner is vital to prevent a spiral into addiction when treating serious mental health disorders.
Vice versa, when treating addiction, you need to be sure that an open and trustworthy support system is available to prevent mental illness development in those in rehabilitation. Unless a support system is available, treatment seems to take progressively longer.
One question this poses, is “Does behavioral addictions, such as phone usage or exercise, exhibit the same level of risk toward mental health disorders?” Though behavioral addictions are not to the diagnostic criterion level of addiction, they still pose immense threat to the quality of life of those already experiencing maladaptive neurotransmission and improper neuroplasticity regarding memory and learning. Phone and social media addictions are more prevalent than ever and exposure to nicotine and other substances are at an all-time high. Behavioral addictions can have damaging effects to physical and mental health to the same degree as substance addictions. If we do not take behavioral addictions to the same extent as substance addiction, we are likely to see an increase in mental illness diagnosis as more and more children grow up in the age of social media.