The snap-crunch of football pads & helmets colliding pulled my attention up from wrapping yet another blanket around myself as I watched my younger brother’s third high school football game of the COVID-modified season while sitting in cold, snow-covered, and socially distanced bleachers with about 30 other player family members. It was 19 degrees Fahrenheit. I was sitting on an inflatable camping sleeping pad with my mom as 22 high school students ran around the field in front of us, each student using the exercise as a somewhat futile attempt to stay warm while endeavoring valiantly to score more points than the other team. Yet, as these athletes gave all of their attention to the game, my mind as a scientist and concerned sibling was drawn to one of the physical perils of competitive varsity football: concussions. As my brother is the star first-string outside linebacker and running back of his team, he ends up involved in tackles on either the receiving or performing side of things on nearly every play.
Concussions are an insidiously common type of mild traumatic brain injury (mTBI) that occurs when the brain rapidly moves within the skull as the head is subjected to rapid acceleration and deceleration. For example – during a football tackle. While advances in protective technology for athletes helps reduce risk, the risk is never zero. This injury can result in both immediate symptoms – pain, ‘seeing stars,’ confusion, headaches – and symptoms lasting weeks – headaches, confusion, and inability to focus. This begs the question, what is happening on a fundamental biochemical level to cause these symptoms?
Inside the brain
Once the initial impact causing the concussion occurs, a cascade of events altering the chemical balance in the brain takes place. First, instead of the typical highly regulated signaling expected in a normal functioning brain, nonspecific depolarization and initiation of axon potentials occur. This causes the release of excitatory neurotransmitters to be widely released throughout the brain at a scale not seen under normal circumstances. This leads to the efflux of potassium ions from the brain and severe ion imbalance, leading to extremely high activity of ATPase, an enzyme responsible for maintaining ion balance in neurons. Since ATPase is powered by ATP, the brain enters an energy crisis trying to restore the ion balance and burns through stored glucose reserves to meet the need. When glucose runs out, the brain switches to other sources of energy which causes lactate to accumulate in the brain. At the same time, the physical injury to neurons results in Calcium entry into the cells. While the ATPase will help rebalance the Calcium entry eventually, in the short-term Calcium entry results in sequestration in the mitochondria. This Calcium imbalance both impairs the mitochondria’s ability to be the “powerhouse of the cell” by interfering with ATP production, further contributing to the brain’s energy crisis, but too much Calcium activates calpain proteins which then initiate apoptosis, or programmed cell death, which results in the dying back of neurons in concussed areas.

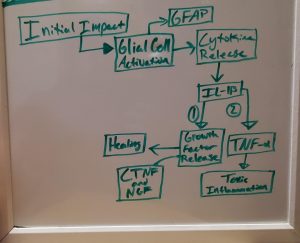
Additionally, scientists are building on this understanding of what happens in concussion by looking at what small chemical messengers that modulate inflammatory responses called cytokines do to change inflammation states in response to injury. After the injury, glial cells called microglia and astrocytes become activated and produce Glial Fibrillary Acidic Protein (GFAP, a biomarker of brain injury) and both pro- and anti-inflammatory cytokines. Due to the existence of both pro- and anti-inflammatory cytokines, teasing apart the differences in how these factors change inflammatory responses is pretty challenging. Interleukin 1 beta (IL-1b) offers an excellent case study in the challenges and opportunities presented by cytokine study.
IL-1b expression patterns after injury show a gradual rise in expression levels, with expression levels directly correlating with the severity of the injury. Interestingly, IL-1b causes the release of ciliary neurotrophic factor (CTNF) and nerve growth factor (NGF), two hormones associated with recovery from concussion. However, IL-1b also stimulates the release of high levels of other inflammation-causing cytokines such as tumor necrosis factor-alpha (TNF-a), which results in toxic inflammation. Therefore, some suggest that interrupting IL-1b after it stimulates growth factor release but before it can stimulate pro-inflammatory cascades may be an effective therapeutic target. Cytokines are incredibly important in regulating neuroinflammation and have both anti- and pro-inflammatory properties, therefore, parsing apart the exact cytokines associated with triggering hyperinflammatory cascades and interrupting their signaling cascades could serve as a therapeutic target in the treatment of concussion.
Clearly, a pharmacologic intervention for concussion treatment is still years away from becoming a reality for athletes. Currently, the best ‘treatment’ for concussions is prevention through educating players, coaches, and parents of all sports on methods that minimize risks of getting a concussion such as proper tackling and running technique, as expertly demonstrated by my brother in his game. While my brother’s team narrowly lost on Friday night, no player got a concussion. So, while not as immediately satisfying as a win, I take solace in the knowledge that through coaching and mentorship, everyone walked away safely.
