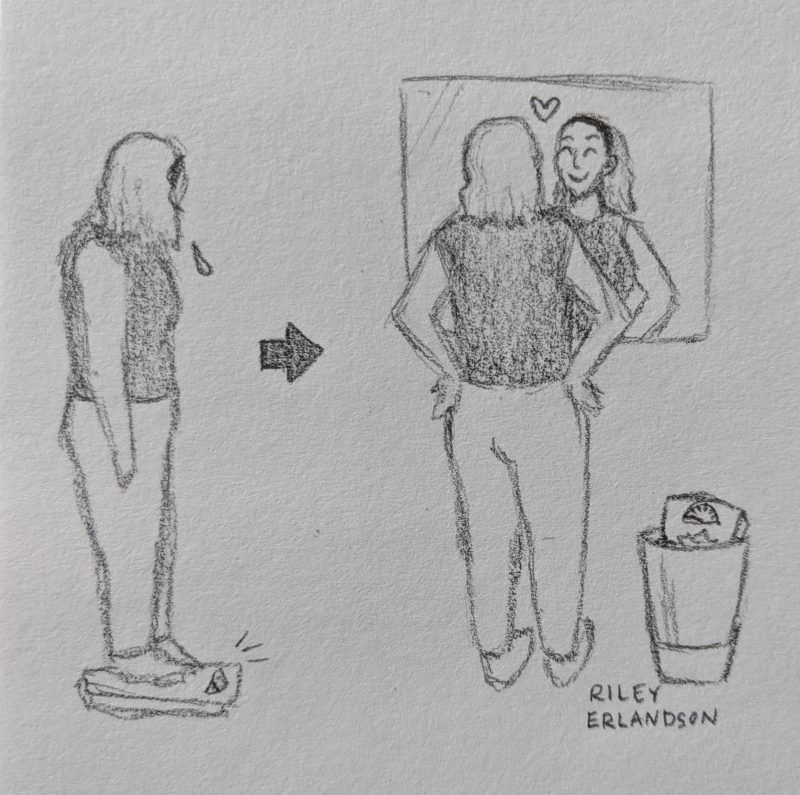
Take a moment to look at the image above. Does something seem to be missing between the person standing on the scale, sad, then looking in a mirror, happy? If you jumped to the same conclusion as me, the answer is “weight loss”! In order to be so happy with their reflection, shouldn’t the person in the drawing have lost dozens of pounds and be smiling at their new, thinner figure?
Not only is it possible to reach the right side of the image without strictly focusing on losing weight, but finding happiness with your body may be even better for you than losing weight. Let’s take a look at obesity and body positivity on the brain!
Controlling Food Intake
First, it’s important to know how the brain normally maintains the appetite balance of being hungry and full. Two key players in this pathway are the hormones leptin and insulin.
Leptin:
- The hormone leptin is released from brain cells (neurons) after food is consumed
- Leptin binds to and activates leptin receptors on the outside of other neurons
- The activated leptin receptor in turn activates proteins called Janus kinases (JAK) which then activate signal transducer and activator of transcription (STAT) proteins
- STAT enters the neuron’s nucleus and causes certain portions of DNA to be transcribed into proteins
- These proteins transfer signals to neurons in the hypothalamus, a central brain region. These signals suppress the orexigenic pathway, which signals that you are hungry, and activate the anorexigenic pathway, which signals that you are full
Insulin:
- The hormone insulin is released from neurons after food is consumed
- Insulin binds to and activates insulin receptors on the outside of other neurons
- The insulin receptors activate a protein called IRS1, which in turn activates a cascade of proteins ending in protein kinase B, also known as Akt
- Akt enters the neuron’s nucleus and causes the FOXO1 protein to leave the nucleus
- When it is in the nucleus, FOXO1 causes DNA to transcribe proteins that suppress STAT activity. Looking back at the leptin pathway, STAT is necessary in the signaling pathway telling your brain that you are no longer hungry. By banishing FOXO1 from the nucleus, the insulin pathway also helps make you feel full
High-Fat Diet = Bad News for Appetite Control
 The way the brain controls appetite and food cravings changes substantially after consuming foods high in fat. Like many “bad” habits, eating high-calorie, high-fat foods can be difficult to stop once you’ve become accustomed to the diet—some even argue that such foods are as addictive as drugs of abuse. The following changes take place in as little as 24 hours after initiation of a high-fat diet (HFD):
The way the brain controls appetite and food cravings changes substantially after consuming foods high in fat. Like many “bad” habits, eating high-calorie, high-fat foods can be difficult to stop once you’ve become accustomed to the diet—some even argue that such foods are as addictive as drugs of abuse. The following changes take place in as little as 24 hours after initiation of a high-fat diet (HFD):
- Saturated fatty acids (SFAs) enter the brain through the bloodstream and bind to TLR receptors
- Now activated, TLR receptors activate a protein called IKK
- IKK goes on to free NF-κB to enter the nucleus, a transcription factor that is normally “blocked”
- NF-κB causes DNA transcription of the SOCS3 gene
- The SOCS3 protein inhibits the insulin and leptin signaling pathways described above, preventing your brain from telling you that you are “full” despite having consumed food
Since the SFAs prevent signaling that makes you feel full, you’re more likely to continue consuming unnecessary food. Not only does a high-fat diet prevent satiation, but it also leads to inflammation in the brain. Proinflammatory cytokines (small molecules inducing inflammation) such as TNF-α are produced following consumption of fatty food and bind to TNF receptors. These receptors activate JNK, a protein that inhibits IRS1, further preventing insulin signaling and compounding the effect of SFAs. Chronic inflammation in the brain, as well as the elevated appetite resulting from SFA consumption, results in bodily inflammation and weight gain.
In summary, eating a high-fat diet leads to brain inflammation and insulin and leptin resistance, resulting in bodily inflammation, increased food intake, and weight gain. But what do weight gain and obesity mean for the individual?
Obesity on the Brain
We’ve looked at how a high-fat diet impacts signaling in the brain leading to obesity. But how does obesity impact the brain and a person’s physical, mental, and emotional well-being?
First, let’s take a brief look at physical health. Obesity is a well-known risk factor for diseases including diabetes and cardiovascular disease. However, there is endless variety among bodies, and it is a simple fact that there is no “healthy weight”. People can be healthy across a wide range of weights, and the number on the scale provides little information about how healthy a person really is. As ingrained as it is in our brains, we must accept the idea that being thin is not equal to being healthy.
Obesity’s effect on mental and emotional health is another story. The modern Western attitude towards beauty informs us that our worth is reliant on our appearance, especially our weight, and that thinness is the ultimate ideal (this is nuanced in the muscular ideal for men, but we’ll loosely use thinness as the opposite of obesity for the purposes of this post). The evidence for the “thin ideal” is nearly endless: people perceived as attractive are more financially successful, the vast majority of models and actresses portrayed as beautiful are thin, and overweight people are stereotyped as lazy.
The societal obsession with thinness often has significant detrimental effects on the mental health of obese and overweight individuals. The constant outright or subliminal messaging that fat bodies are not wanted, not ideal, and worth less than thin bodies can cause serious stress in people who feel they don’t fit the “correct” beauty image. Not only is constant stress and negative body image clearly bad for mental health and quality of life, but elevated rates of cortisol, the stress hormone, can also further interrupt the appetite regulation pathway discussed above, leading to further weight gain and often compounding stress and body dissatisfaction.
Body Positivity
 The body positivity movement seeks to combat the stigma around bodies that don’t fit the thin ideal or other aspects of the Western beauty standard. By promoting acceptance of all body types, body positivity advocates for love and shifting the idea that a person’s intrinsic worth is wrapped at all in their physical appearance. And body positivity is not just for overweight and obese individuals: a jaw-dropping 2% of women report being “totally happy” with their bodies. With such rampant dissatisfaction with our bodies, we can all benefit from a shift towards body positivity.
The body positivity movement seeks to combat the stigma around bodies that don’t fit the thin ideal or other aspects of the Western beauty standard. By promoting acceptance of all body types, body positivity advocates for love and shifting the idea that a person’s intrinsic worth is wrapped at all in their physical appearance. And body positivity is not just for overweight and obese individuals: a jaw-dropping 2% of women report being “totally happy” with their bodies. With such rampant dissatisfaction with our bodies, we can all benefit from a shift towards body positivity.
Critics of the movement claim that body positivity simply excuses obesity and ignores the health risks that go along with it. However, studies have shown that body positivity movements have nothing but positive effects on health: individuals who think positively about their physical appearance tend to have better mental health and are more likely to take care of themselves. By first destigmatizing obesity and fat bodies, we can send the message that all bodies are beautiful and worthy of love, and thus have a strong foundation from which to build healthy eating and exercise habits for the purpose of health rather than adherence to thin beauty standards.