
Good things in life often come with risks. Sports are no exception; lots of physical, social and psychological benefits can be gained from engaging in sports, but many of them come with a risk of injury to the brain. A person can get a concussion through a variety different avenues, and sports are one of the most common- other ways include falling, vehicle accidents and military combat, or anything else that causes physical trauma to the head. Given the serious impact that concussions can have on our brain’s functioning, any steps to minimize this risk should arguably be taken. This may not only include further research and improved screening, but dietary supplements as well.
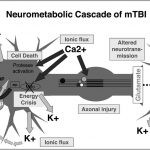
Medically speaking, concussions are called Traumatic Brain Injury (TBI) and are most directly caused by biomechanical force (considered the first injury phase) that disrupts the brain’s functioning (the second injury phase). The second injury phase involves the consequences of the first injury phase, and consists of many detrimental effects. For example, TBI has the ability to cause increased axon permeability and damaged neurofilaments in the brain, both of which may lead to axon dysfunction or disconnection. Much of this dysfunction builds upon itself as a cascade of events; initial ionic flux and glutamate release caused by the biomechanical force can result in increased energy demands and a period of metabolic crisis, leading to even more dysregulation. Inflammatory changes can also be triggered by TBI, possibly resulting in cellular injury and immunoexcitotoxicity.
The Western medical system typically revolves around a “one problem, one solution” framework, but given how many ways our brain can be affected on a cellular level by TBI, a treatment that targets multiple aspects may be necessary. This is where dietary supplements come in. Omega-3 fatty acids (also called n-3FAs) may be able to fulfill a role like this, since they have the ability to affect all major mechanisms of TBI second injury phase through neuroregeneration, neuroprotection, and neuroinflammation.
There are three types of omega-3 fatty acids used by the human body: ALA, EPA, and docosahexaenoic acid (DHA), but the majority of omega-3 fatty acids in the brain are DHA, functioning as a main ‘ingredient’ in central nervous system membranes. Increasing the amount of DHA present in membranes can promote neurite growth, branching, and synaptogenesis which support regeneration. In addition, protective molecules such as neuroprotectin D1 are derived from DHA in response to cellular stress. Since DHA is anti-inflammatory by nature, and anti-inflammatory resolvins are also derived from DHA, it may help to reduce neuroinflammation caused by TBI as well.
Surprisingly, there is currently a complete lack of randomized clinical trials (RCTs) for use of omega-3 fatty acid supplements as a treatment for TBI. Evidence is largely anecdotal so far, but a few connected case studies suggest strong treatment potential. In 2010, a teenager got into a car accident and suffered severe TBI with diffuse axonal injury that the head neurosurgeon thought would be lethal. By day 10, he was in a permanent vegetative state. Based on a previous treatment success for a man who had survived a mining explosion, the teenager was given 20g of n-3FA daily. He was weaned off the ventilator by day 21, and went home 4 months later. Then, a mother with an 8-year old daughter who had been in a comatose condition for 82 days from brain injury saw this story on TV- she asked her doctors to try the same treatment, and her daughter was discharged one month later.
Of course, a benefit vs. risk analysis should also be considered regarding the use of fatty acid supplements for treatment of TBI. Side effects, if present, are generally mild and short term, with the only other risk cited by the National Center for Complementary and Integrative Health being a possible association with prostate cancer (studies have had conflicting findings). The average Western diet is highly pro-inflammatory, and it is likely that many of us have a deficiency of omega- 3 fatty acids that could increase susceptibility for TBI. For this reason, supplementation may not be a bad idea for prevention as well as treatment, or even to support our brain’s functioning in general.
While there are no published RCTs that examine treatment potential of omega-3 fatty acids to date, three (1, 2, 3) new trials have been in progress since 2019! This should help clarify both the safety and efficacy of these supplements, possibly paving the way for their incorporation into treatment plans and offering added protection from damage to our brains. This, in turn, this could help reduce the risk of sports that many people love.