 By Hannah P.
By Hannah P.
How do we feel pain?
When we feel pain sensory receptors in our skin send a message via nerve fibres, A-delta fibres and C fibres, to the spinal cord and brainstem and then onto the brain where the sensation of pain is registered, the information is processed and the pain is perceived. Fast pain is transported from A delta fibers while slow pain from C fibers.Examples of A delta fiber pain are sharp, prickling and acute pain and C fibers are slow, throbbing, aching chronic pain.
What is the pathway for pain?
In short form pain starts at nociceptors –> Primary afferent sensory fibers –> Dorsal root ganglion –> Na channels allow depolarization through axons –> Dorsal Horn of spinal cord –> Second order neurons –> Brain.
The General Pain Pathway
Within the pain pathway there are 3 orders of neurons that carry action potentials, signalling pain. First-order neurons are pseudounipolar neurons which have cell bodies within the dorsal root ganglion. They have one axon which splits into two branches, a peripheral branch (which extends towards the periphery) and a central branch (which extends centrally into the spinal cord/brainstem). Second-order cell bodies of these neurons are found in the rexed laminae of the spinal cord, or in the nuclei of the cranial nerves within the brain stem. These neurons then decussate in the anterior white commissure of the spinal cord and ascend cranially in the spinothalamic tract to the ventral posterolateral (VPL) nucleus of the thalamus. Third-order the cell bodies of third-order neurons lie within the VPL of the thalamus. They project via the posterior limb of the internal capsule to terminate in the ipsilateral postcentral gyrus (primary somatosensory cortex). The postcentral gyrus is somatotopically organised. Therefore, pain signals initiated in the hand will terminate in the area of the cortex dedicated to sensations of the hand.
How do we react to pain?
This can lead to two different responses, fight or flight. In response to the pain stimulus the brain overall increases in “fight or flight” arousal.
– increased sympathetic tone
– increased catecholamine release
– increased metabolism & oxygen consumption (via hypothalamus)
How can you treat pain?
There are many ways an individual can help reduce pain and manage it. Some people will say to get plenty of rest, distract yourself, or participate in light exercise. However, what happens when these tips don’t help with the pain? Many people reach for pharmaceutical mechanisms to treat what they are experiencing from ibprohpen to different opioids. This occurs by inhibiting nociceptors and dorsal horn pain transmission.
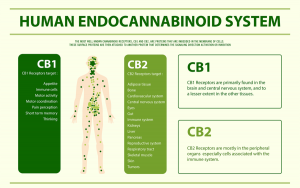
What are CB1 and CB2?
CB1 are receptors found primarily on the presynaptic membrane of neurons, ubiquitous. It is coupled to G proteins, causing inhibition of adenylyl cyclase, influencing numerous transcription factors and potassium channels. While CB2 are receptors which are more localized, specifically to immune cells. Both CB2 and CB1 receptors on mast cells participate in the anti-inflammatory mechanism of action of cannabinoids.
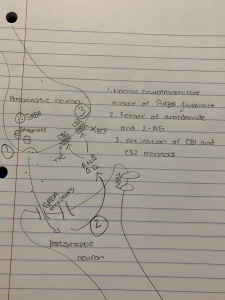
How is CB1 involved in pain management?
The CB1 receptor is distributed throughout the nervous system. It mediates psychoactivity, pain regulation, memory processing and motor control. CB1 is a presynaptic heteroreceptor that modulates neurotransmitter and neuropeptide release and inhibits synaptic transmission. Activation of CB1 results in the activation of inwardly rectifying potassium channels, which decrease presynaptic neuron firing, and in the inhibition of voltage-sensitive calcium channels that decrease neurotransmitter release. Allosteric modulators of the CB1 receptor bind to a distinct site apart from the orthosteric site and produce conformational changes in the receptor, thereby altering the potency of the ligand when it binds to the receptor. No effect in the absence of ligand binding. So, CB1 positive allosteric modulators would be expected to enhance the pain relieving effects of endocannabinoids, but with limited side effects. ZCZO11 reduced neuropathic pain and inflammatory pain without development of tolerance or occurrence of psychoactive side effects.