
Insulin
Insulin is a peptide hormone with numerous functions in the body, the most common of which is to control glucose levels. Insulin acts differently in the pancreas, liver, bones, and so on than it does in the brain. Insulin regulates neuron growth, survival, differentiation, and communication in the brain. So, what happens when insulin is not properly regulated?
Insulin resistance
This is a condition in which the body and brain are unable to use glucose as an energy source effectively. The ability to be insulin sensitive is lost, and as a result, glucose absorption by brain cells is compromised. Insulin regulates brain metabolism and overworked insulin receptors cause brain cells to die. Chronic oversupply of glucose to brain cells causes the cells to overwork in order to metabolize the excess fuel, eventually giving up and committing suicide via a process known as apoptosis.
This has an effect on neuro communication in the brain because glucose is what the cells require to function properly. At this point, the brain is essentially starving. There is an abundance of glucose but no way to use it.
High carb content diets, like the typical American diet promote chronic and prolonged blood sugar spikes. This prolonged glucose overdose starves the brain and later manifests itself as cognitive impairment. Cognitive ability is directly proportional to energy supply to the brain.
Diabetes
It is critical to distinguish between type I and type ii diabetes. We lack the ability to produce insulin in type I diabetes, so glucose levels in our bodies are high. In type II diabetes, however, insulin is present, but it is excessive, and our cells become resistant to it, raising glucose levels to dangerously high levels. When we think of diabetes, we usually think of the heart, kidneys, and pancreas as the most affected organs. But what about the brain?
Diabetes accelerates brain aging, which, as we know, causes neurodegenerative diseases such as Alzheimer’s. Blood flow to the brain is reduced in diabetic patients, causing neuron damage. These neurodegenerative changes occur at a much earlier stage. Diabetes also impairs byproduct metabolism in patients, resulting in the buildup of undesirable substances such as amyloid plaques and neurofibrillary tangles found in Alzheimer’s disease.
In diabetes, people have smaller brain volume of the frontal and temporal lobes due to brain atrophy triggered by excessive cell apoptosis.
Inflammation and Alzheimer’s Disease
When most people hear the words Alzheimer’s disease, they envision plaques and tangles. We know that amyloid plaques and neurofibrillary tangles are major indicators of neurodegenerative disease, most notably Alzheimer’s disease.
Plaques cause one of three problems in the brain:

- Disruption of neuron communication by acting a physical barriers in synapses
- Trigger inflammation through the intervention of the immune system
- Increased risk of hemorrhage in blood vessels through amyloid angiopathy
Tangles form when plaques accumulate outside of neurons. Tangles cause significant disruption in the cell’s transport system, the microtubules.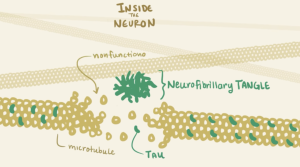
Tangles, combined with plaque buildup, eventually cause the cells to die via apoptosis. This explains why reduced brain atrophy, a condition caused by too much cell death in the brain, is a major symptom of Alzheimer’s disease.
If this blog is to be of any use to you, I want you to be able to link insulin to the formation of plaques and tangles, and, in the larger picture, Alzheimer’s disease.