Treatment of Schizophrenia
Schizophrenia is a very consequential mental illness, its effects can alter how someone can think, feel, and act. Often it tends to go untreated. According to WHO only 31.3% of people with schizophrenia get treatment from specialists. You might ask yourself “if help is offered, why don’t people get the help?” Well, it isn’tthat easy.
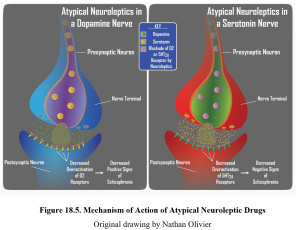
Pathways Targeted by Anti-Psychotics.
There are four major pathways that anti-psychotics can target. The mesolimbic pathway is altered because people with schizophrenia have too much dopamine. This can cause satisfaction, emotions, and thoughts not be the same. Anti-psychotics lower dopamine transmission. The mesocortical pathway controls cognition and reward processing. The nigrostriatal pathway controls movement can cause things like tics. The tuberoinfundibular pathway gets effected by the high dopamine levels by causing too much prolactin. This causes the hysteria and hallucinations.
Most anti-psychotics target dopamine receptors in the brain. They block the receptors so that dopamine isn’t processed that cause the symptoms of schizophrenia. Which again you still might be asking yourself “why don’t they take the treatment?”
What Happens at These Receptors?
Antipsychotics cause D2 receptors to inhibit the enzyme Akt. Akt is responsible for the phosphorylation of GSK3β. Antipsychotics cause the GSK3β to be inhibited.
In medicated schizophrenia patients compared to ones not treated with an anti-psychotic, non- medicated had 5.8% more active D2 receptors.
The dopamine D2 receptor releases clozapine and quetiapine (both are commonly used to treat schizophrenia) more rapidly than it do any of the other antipsychotic drugs.
Perceived Effects of Anti-Psychotics
It inhibits dopamine transmission; it can cause people’s lives to become dull. Sadly, it seems to be a hit or miss acting. Yes, anti-psychotics can stop extreme symptoms, but it also inhibits dopamine transmission for typical everyday life. There are things in life that naturally produce dopamine you don’t even think of. Any sort of action or activity that gives you satisfaction gets dulled while on anti-psychotics. I am not sure about you, but simple things even like selfcare Sunday night to get ready for the upcoming week is something I look forward too. I get so much satisfaction from doing a facemask and crawling into a freshly washed and made bed. While on anti-psychotics, that wouldn’t be rewarding. It can cause people to be a lot less motivated.
Another factor that often gets mentioned is the stigmatism about taking “anti-psychotics.” Think of the word means, I personally think “undoing-the delusion.” As much as I don’t want to say it, but in society it is made to seem if you take anti-psychotics you are “crazy.” Which I can understand how that stigmatism happened due to some cases of symptoms. Yet, if we all had the same unbalance within ours brains we’d be “crazy” too. At the end of the day, we don’t and we can’t undo it for others that do. So truly tagging such negative ideals to something so impacting such a schizophrenia is unfair. Those that deal with it are already just trying to deal with impacts.
The Future of Treatment
As time goes on so does research, more suitable treatment plans are being investigated. A middle ground, not an all or nothing strategy is the goal. Recently an oral compound SEP-363856, has been studied as a medication for schizophrenia. A 2020 study posted to the New England Medical Journal has studied SEP-363856. It isn’t a D2 inhibitor, but an agonist at TAAR1. TAAR1 is a G-coupled protein receptor that has been shown to alter dopamine, serotonin, and glutamate activity. It is currently in phase 3 of clinical testing. Most studies were short, (around 4 months long) yet have shown positive results. The only one thing negative thing I can find so far on this drug is that it may be suitable for mild Schizophrenia cases. Another note on treatment plans I found is that majority of treatment is being done to treat Schizophrenia. There isn’t much being done or real definitive answers to help the physical brain matter of people with Schizophrenia. That not too much can be done for preventative care.
A Peak into Schizophrenia
I found this little youtube video that has a young boy with schizophrenia and his treatment team. I think it is worth the watch. You can read as much as you want to try to understand what symptoms may be like, this video helps me see what it is somewhat like going off of this real life story. It also mentions another treatment plan that is in clinical trial, this one focuses on the auditory system. Which personally blows my mind that so far it seems to be effective. It doesn’t effect dopamine pathways which cuts out the bad effects of anti-psychotics. Instead it helps with auditory hallucinations. It targets the processings within the brain.
Sources
https://www.who.int/news-room/fact-sheets/detail/schizophrenia
https://pubmed.ncbi.nlm.nih.gov/32294346/
https://psychopharmacologyinstitute.com/publication/the-four-dopamine-pathways-relevant-to-antipsychotics-pharmacology-2096
https://www.nature.com/articles/s41398-021-01331-9#:~:text=SEP%2D363856%20is%20a%20trace,for%20the%20treatment%20of%20schizophrenia