Artstract from DALL-E2 created by Kailee Vigen
Introduction to Addiction
Millions of Americans ages 12 and older struggle with addiction. These substance problems can exist at any age and may be influenced by one’s social environment, development or upbringing, cognitive function, or genetics. Addiction is often described as a disease, involving physiological and brain alterations that are incredibly difficult to combat or reverse, especially when treatment options are still underdeveloped and not of easy access. So, what is really going on with addiction, and is there a way to universally and effectively treat it?
Drugs of abuse are very diverse in that they each elicit distinct combinations of behavioral and physiological effects. But, these drugs also cause similar effects to each other – they are all rewarding which leads to addiction and they also produce negative symptoms in withdrawal. The question is if there are common molecular and neural pathways of these drugs of abuse that elicit these shared rewarding and addicting actions. And if there are, it could be key for finding effective treatment!
Neurology of Addiction
The ventral tegmental area (VTA) and nucleus accumbens (NAc) circuit of the limbic system is the primary reward pathway in the brain. All drugs of abuse converge on this VTA-NAc pathway which includes dopaminergic neurons in the VTA targeting the NAc which activates dopaminergic transmission in the NAc, producing dopamine-like effects. Regions of the limbic system (hippocampus, amygdala, hypothalamus, frontal cortex) also play a large role in natural addiction reward. It is speculated that there are shared reward pathways and similar anatomical brain abnormalities between drugs of abuse and natural addictions.
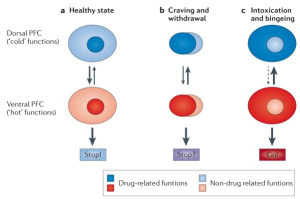
Hypofrontality is the loss of executive function (self-control, self-monitoring, planning, judgment, etc.) in the prefrontal cortex (PFC) which exists in addicted individuals. Neuroimaging studies have revealed a pattern of PFC dysfunction in drug-addicted individuals involving decreased input from the “cold functions” (non-drug related, “good” judgment) of the dorsal PFC and increased input from the “hot functions” (drug-related, impulsive judgment) of the ventral PFC as illustrated by the arrows in the figure below. This decreased function contributes to the compulsiveness, cravings, and loss of self-control seen with addiction.
Treatment of Addiction
With the knowledge of shared mechanisms of drugs of abuse and natural rewards, there are safety concerns regarding universal treatment. Thus far, there is no treatment aimed at common drug mechanisms for a range of drug addictions. Current treatments include prescribing drugs such as methadone, suboxone, narcan, or cameral. However, these drugs for treating addiction are also addicting themselves, often making this course of treatment not sustainable.
In a more promising, preventative light, neuroimaging could be used to detect abnormalities in the PFC, as discussed previously, before addiction even occurs! It has been found that PFC dysfunction precedes addiction, leaving some individuals more susceptible to addiction. Knowing that addiction is influenced by social environments, genetics, and certain developmental circumstances, those who have been around addicted individuals in their upbringing or have familial ties to addiction could benefit from early neuroimaging. Having the ability to identify such abnormalities in an individual early on could be beneficial in providing drug addiction preventative efforts!
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3462342/
https://pubmed.ncbi.nlm.nih.gov/16251986/
