What is obesity?
Obesity is considered to be an excessive or abnormal buildup of fat that causes risk to one’s health. Body mass index is how this is normally determined with people over 25 being labeled as overweight (Fig. 1). However, BMI is not always the most accurate representation because body mass can also be muscle weight instead of fat. For example, a body builder will obviously weigh more because of their muscle, but this does not mean they are obese. Society seems to have a stigma associated with the term “obese”, but the brain functioning behind this need to eat is important to understand. Furthermore, the problems with obesity do not stop there; the after-effects of the condition can include type 2 diabetes, dyslipidemia, cardiovascular diseases, and neurodegenerative disorders.
The hypothalamus and Obesity
One of the main components that plays a role in obesity relates to the hypothalamus, which is known for its role in homeostasis. The hypothalamus controls metabolic feedback and regulates energy homeostasis, so it has important influences on feeding behavior and energy spending. How does the hypothalamus do this? It is able to sense and integrate feedback from adipostatic hormones that are responsible for circulation of nutrients to adipose tissue. Specifically, leptin and insulin directly affect the ARC of the hypothalamus that works with energy homeostasis. However, neuronal inflammation and insulin and leptin resistance of the ARC neurons disrupts the metabolic feedback loop, which causes an increase food intake and body weight gain. Overconsumption of fat-rich diets changes the feedback sent to leptin and insulin, causing hypothalamus inflammation.
Further Inflammation caused by Saturated Fatty Acids
Inflammation can be worsened with other factors as well. One factor that plays a role in this are cytokines; they are small proteins that are vital in controlling the growth and activity of other cells. However, during diet-induced obesity, cytokines are overactivated, which farther leads to more hypothalamic inflammation. Saturated fatty acids can modulate neuronal control of energetic homeostasis as well. These fatty acids can cross the blood brain barrier, accumulating in the hypothalamus and triggering inflammatory signaling cascades.
Other eating Disorders- Serotonin and Dopamine
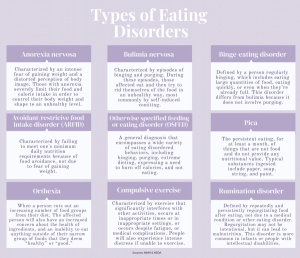
We know the background on the homeostasis imbalance that occurs for irregular feeding. Then, what are the eating disorders that can occur from different brain imbalances? First of all, eating disorders are serious health conditions that affect both your physical and mental health. These conditions include problems in how you think about food, eating, weight and shape, and in your eating behaviors (Fig. 2). These symptoms can affect your health, your emotions, and your ability to function in important areas of life.
Dopamine and serotonin also have been linked to eating disorders like anorexia. Dopamine is a chemical involved in weight, feeding behaviors, reinforcement, and reward. Since serotonin is involved with satiety and dopamine is associated with the brain’s reward system, altered receptor activity may explain why people with Anorexia have reduced hunger signals and alterations in their food reward system. Dopamine has also been linked with binge eating because it has a role in food cravings, decision making, executive function, and impulsivity, as well as its functional associations with these risk factors.
Conclusion
Obesity has a negative connotation often associated with it in society. However, it is important to understand the complexity behind what causes obesity. Obesity is not the only eating disorder that impacts so many lives; rather, there are many others as well that are caused by the changes in our brains. The hypothalamus, specifically, is often affected because of its role in homeostasis. The reward system is also crucial in how we eat and see food. The complexity behind eating is great and not an easy obstacle to overcome.
Citations:
- Jais, A., & Brüning, J. C. (2017). Hypothalamic inflammation in obesity and metabolic disease. Journal of Clinical Investigation, 127(1), 24–32. https://doi.org/10.1172/jci88878
- Steiger, H. (2004). Eating disorders and the serotonin connection: State, trait and developmental effects. Journal of Psychiatry and Neuroscience, 29(1).
- The Editors of Encyclopaedia Britannica. (2008, December 3). Body mass index (BMI). Encyclopedia Britannica. https://www.britannica.com/science/body-mass-index
- Ward-Zaragoza, M. (n.d.). Eating Disorder Awareness Week explained: Support, resources, symptoms. Buena Speaks. Retrieved April 29, 2023, from https://buenaspeaks.org/6407/features/eating-disorder-awareness-week-explained-support-resources-symptoms/
- WHO, W. H. O. (2020, February 21). Obesity. World Health Organization: WHO. https://www.who.int/health-topics/obesity
