
What Is Alzheimer’s Disease?
Alzheimer’s disease (AD) is a neurological condition that causes millions of people to suffer from cognitive deficits. There is not a set answer for treating and preventing the disease as the pathology is still not completely understood, however, there are a few different theories pertaining to the development of the disease. One of the theories is that dysfunction within the insulin signaling pathway is responsible for the pathogenesis of Alzheimer’s disease. [1]
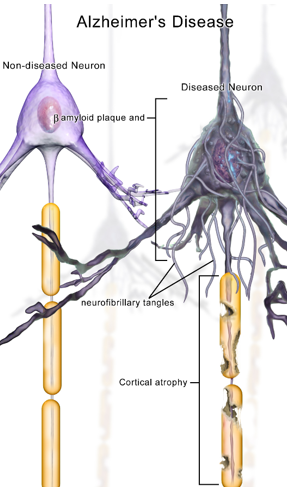
The two main biomarkers of Alzheimer’s disease are β-amyloid plaques and neurofibrillary tangles (NFT). NFTs are the result of tau proteins becoming hyperphosphorylated, causing them to clump together and disrupt the function of the microtubules. When the microtubules are not working properly, the neuron cannot work properly. β-amyloid plaques are formed by amyloid precursor proteins (APP) and can compete with insulin in binding to insulin receptors, causing dysfunction. Both NFTs and β-amyloid plaques have a role in insulin resistance. [1]
While insulin was once thought to not have any prevalence in the brain, we now know that there are concentrations of insulin and insulin receptors in some brain regions. Insulin can be synthesized in the brain and can also cross the blood brain barrier. It has a regulatory role in neuroprotection. Insulin also plays a role in memory and learning and has been shown to regulate the accumulation of amyloid β. Some studies have found that dysregulation of glucose metabolism can lead to memory loss and dementia symptoms of AD. [1]
AD and the Insulin Signaling Pathway
There are multiple components throughout the insulin signaling pathway that could be possible sites for AD pathogenesis. Irregularities and dysfunctions regarding these components can lead to the development of AD symptoms including dementia and deficits with working memory and learning. For example, mTOR is a protein involved in the PI3K pathway triggered by growth factors to regulate metabolic activity. Another example is that when GSK-3β is phosphorylated, it facilitates the formation and accumulation of β-amyloid plaques as well as the accumulation of phosphorylated tau proteins leading to NFTs. Amyloid β has also been found to activate GSK-3β which can lead to even more phosphorylated tau proteins. [1]
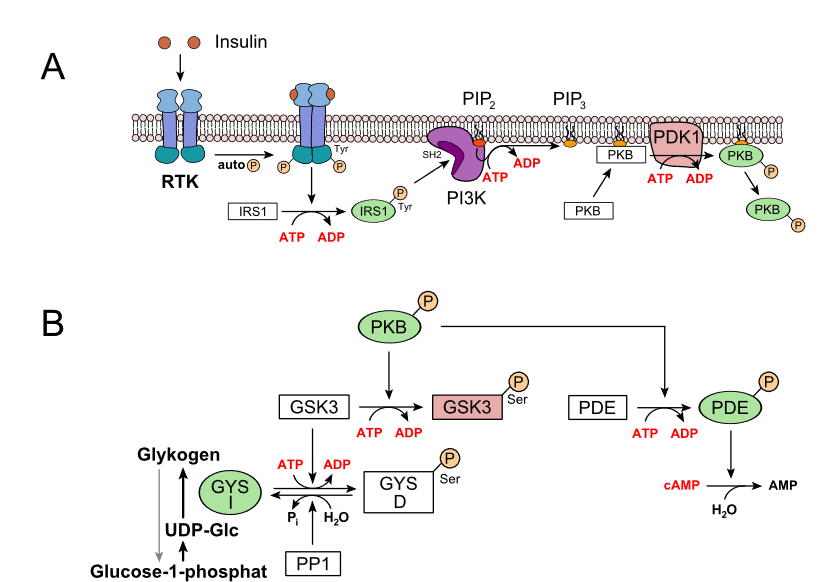
The article Insulin signaling and AD described an AD mouse model that showed evidence of irregularities in mTOR signaling and that phosphorylated mTOR was elevated in AD subjects. Several of the dysregulated molecules lead to the production and accumulation of β-amyloid plaques and neurofibrillary tangles which are key factors of Alzheimer’s disease. [1]
Is Insulin Resistance Responsible for AD?
While there is substantial evidence for insulin resistance being a probable cause to Alzheimer’s disease, there are still some things researchers need to evaluate. Insulin resistance has been shown to increase other things that have been hypothesized to contribute to the development of Alzheimer’s. These things include oxidative stress, the production of cytokines, and process leading to cell death. Insulin resistance may be a great theory as to why neurological diseases like Alzheimer’s occur but may also just influence other forces that contribute to the disease. [1]
Lifestyle as Prevention
Alzheimer’s disease is not the result of one sole issue. Insulin resistance can begin in the body through a variety of circumstances. Diabetes mellitus is a more commonly known form of insulin resistance, but can also develop from an excessive caloric intake and/or a high-fat diet. Insulin resistance can also develop due to physical inactivity. Making a conscious effort to maintain a healthy lifestyle has a lot of benefits regarding the prevention of neurodegenerative diseases like Alzheimer’s. [2]
[1] A. Akhtar and S. P. Sah, “Insulin signaling pathway and related molecules: Role in neurodegeneration and Alzheimer’s disease,” Feb. 21, 2020. [Online]. Available: https://doi.org/10.1016/j.neuint.2020.104707
[2] U. Pagotto, “Where Does Insulin Resistance Start?: The brain,” Diabetes Care, vol. 32, no. suppl_2, pp. S174–S177, Nov. 2009, doi: 10.2337/dc09-S305.