PHOTOPHOBIA
Although photophobia literally means to have a ‘fear of light’, it actually refers to pain or discomfort caused by light exposure.
This is a neuro-ophthalmological disorder, which means the optic nerves are affected along with the brain. So, even though eye disorders commonly involve light sensitivity, photophobia can be caused by a variety of things.
Photophobia is one of the most common ocular conditions that occur with tension headaches, migraines, or TBI’s (Traumatic brain injury’s).
TBI’s (Traumatic Brain Injury)
Photophobia is one of the most common symptoms of concussions and TBI’s. TBI produces cognitive symptoms such as dizziness, vertigo, nausea, irritability, cognitive delays, and vision related symptoms to light-sensitivity. About 40% of individuals with brain injuries experience sensitivity to light. But, Light sensitivity can show up post-concussion or 6 months to even years after the concussion occurred.
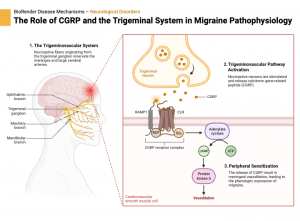
Cranial Nerve 5- trigeminal CN V
The star of the show in pain processing within the head and eyes is cranial nerve five (the trigeminal nerve), the largest cranial nerve. The trigeminal nuclei and nerves play a crucial role in moderating pain, particularly in the eyes and head.
The trigeminal ganglion houses the ophthalmic branch (V1), which is primarily responsible for transmitting pain signals from the cornea, conjunctiva, sclera, and uvea–these structures are extremely sensitive to pain.The trigeminal nerve is an essential player in processing sensory information from the face and head.
When pain is experienced, it is often linked to the release of (CGRP) Calcitonin gene-related peptide. This peptide is released in response to stimulation from the trigeminal nerve and plays a critical role in the pain signal transmission to the brain. CGRP is located in the trigeminals ganglion, which is triggered by stress, brain vessels, and or inflammation.
What Causes Photophobia in TBI’s?
With TBIs, photophobia (light sensitivity is usually caused by injury to the thalamus, preventing it from getting oxygen. This disruption impairs its function, leading to heightened sensitivity to light. But, in a TBI light sensitivity could mean dysregulation in one or multiple areas of the brain. The problem isn’t always isolated.
This creates a symptom cascade, where an issue in one area can trigger problems in others area. Dysfunction in the visual process could possibly affect focus, balance, or overall symptoms which creates a harder recovery process.
Thalamus
The thalamus is in charge of relaying sensory information to the brain. It is crucial for directing sensory signals, when a TBI occurs the process is disrupted.
The dysregulated mechanism that occurs is neurovascular coupling, which happens in the brain and retina. When communication pathways are faulty, neurons and blood vessels start malfunctioning and there isn’t always enough oxygen to be used.
As a result, patients experience light sensitivity in order to minimize their sensory overload and are recommended to stay in dark rooms. This reduces the amount of visual input letting the brain rest and recover
Autonomic Nervous System
The autonomic nervous system (ANS) is in charge of involuntary system, which involves functions like heart rate, breathing, and digestion Within light sensitivity, pupils dilate more than needed in a post concussion scenario causing exposure to light causing sensitivity. The dysregulation in the ANS causes abnormal pupil responses.
Vestibular System
The vestibular system involves the inner ear, sight, and touch. Dysfunction in this area causes the body to become off balance, leading to dizziness and vertigo. When the Vestibular system and visual system disagree, this increases optic sensitivity–which in turn creates an overload of sensory information.
Superior Colliculus
The superior colliculus is in charge of visual mapping and coordination, aiding in detecting and locating visual and audio stimuli. This contributes motor functions to orient the head and eyes toward or away from a stimulus. This is described as a looming stimulus which can be perceived as a threat from an object moving towards you and initiates a response from fear. For example a snake would be processed in the superior colliculi and initiate a motor response which would orient an individual away from the snake, as the brain perceives it as dangerous. This can occur without eye movements as an instinct response.
Photophobia in TBI’s
Therefore, Photophobia in TBI’s is involved in several structures including thalamus, ANS, vestibular system, and superior colliculus. Light sensitivity is commonly found as a system of ocular disorders, in TBI’s it is a neurological dysfunction. This dysfunction occurs by dysregulation in sensory processing, such as lack of oxygen supplied to the brain or the miscommunication between sensory and visual pathways which increase light sensitivity.
CN V, The trigeminal nerve is responsible for transmitting these pain signals after TBI occurs. With the involvement of the CGRP pathway, the trigeminal nerve is responsible for a cascade of symptoms depending on the brain structure that is affected. Understanding photophobia in TBI’s in important for deciding treatment, limiting sensory input, and understanding multi-system dysfunction.
Footnotes:
Abusamak, Mohammad, and Hamzeh Mohammad Alrawashdeh. “Post-Concussion Syndrome Light Sensitivity: A Case Report and Review of the Literature.” Neuro-Ophthalmology 46, no. 2 (n.d.): 85–90. https://doi.org/10.1080/01658107.2021.1983612.
n J., and Matilde Inglese. “The Role of Thalamic Damage in Mild Traumatic Brain Injury.” Journal of Neurotrauma 33, no. 2 (January 15, 2016): 163–67. https://doi.org/10.1089/neu.2015.3965.