Concussion protocols in sports are designed to protect athletes and prevent long-term brain damage. However, many athletes are still returning to play before they are fully recovered. Current protocols rely heavily on self-reported symptoms and subjective assessments, which can lead to players downplaying their injuries in order to compete.1 As research determines the long-term risks of concussions, it’s time to reevaluate how we assess and manage these injuries.
The Limitations of Current Concussion Protocols
Concussion protocols vary across sports and organizations, often including sideline assessments, symptom checklists, cognitive testing, and gradual return-to-play (RTP) guidelines.1 However, key problems remain:
- Self-reported symptoms are unreliable – Studies show that symptoms alone do not accurately identify all concussed athletes or determine full recovery.1 Athletes may underreport symptoms to avoid being sidelined.
- Subjective assessments create inconsistencies – Tests like the Sport Concussion Assessment Tool (SCAT) rely on athlete-reported symptoms, which can be influenced by external pressures and personal motivation to compete.
Because of these limitations, athletes may unknowingly return before their brain has fully healed, increasing the risk of repeat concussions and long-term consequences.
The Effects of a Concussion
Concussions can trigger a wide range of effects within the brain. Figure 1 illustrates the complex cascade of events that follow this type of injury.2 The process begins with an influx of cations, such as sodium and calcium. This forces neurons to increase energy production in the form of ATP. This increased activity quickly reduces the neuron’s resources, leading to an energy crisis.
As the cell works to restore this cation balance, more issues occur. The excessive production of ATP generates oxidative stress, which compromises the integrity of the cell membrane.3 The influx of calcium activates proteases enzymes that break down proteins which can result in protein loss within the cell. These disruptions can lead to axonal injury and cell death.2

Figure 1. Neurometabolic cascade of events that can occur after a concussion.2
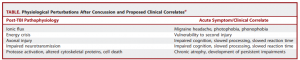
This cascade of events within the neuron can lead to a variety of symptoms. Table 1 provides a detailed overview of these symptoms and their connection to the affected pathophysiological processes.
Table 1. Symptoms related to their affected pathophysiological process.2
A more detailed explanation of the cascade of effects caused by concussions can be found in this article.
The Science of Recovery and the Impact of Repeat Injuries
While it may seem that the symptoms are gone, the brain remains vulnerable. Returning too soon can lead to:
- Second-impact syndrome – A condition where a second concussion occurs before the first has healed.
- Chronic traumatic encephalopathy (CTE) – A degenerative brain disease linked to repeated head trauma.
- Long-term cognitive impairment – Problems such as memory and behavioral issues.
Research confirms that even after successful completion of a graduated RTP protocol, athletes may still be at a higher risk of neurological and musculoskeletal injuries.1 More measures are needed to track recovery.
Improving Concussion Protocols
Advancements in brain imaging and neurocognitive research can offer promising ways to enhance concussion management. Key improvements for concussion protocols could include:
- Objective diagnostic tools – Tests like biomarker analysis, diffusion tensor imaging (DTI), and functional MRI (fMRI) can provide more accurate assessments of brain recovery.2
- Stronger return-to-play goals – Rather than relying solely on self-reports, RTP should incorporate standardized neurocognitive assessments that detect lingering impairments.
- Education – Athletes, coaches, and medical professionals should prioritize brain health over competition. RTP decisions should be made with long-term well-being in mind.
Beyond Sports: Why Better Concussion Protocols Matter for Everyone
Concussion management isn’t just a concern for professional athletes. It affects youth sports, military personnel, and everyday individuals. Improved protocols could:
- Protect young athletes from long-term cognitive issues.
- Help military veterans reduce the risk of neurodegenerative diseases.
- Improve workplace and recreational injury management to prevent lasting damage.
If we continue relying on outdated or lenient concussion protocols, are we prioritizing competition over health? With advancements in science and technology, we have an opportunity to develop more accurate, evidence based concussion management strategies. It’s time to rethink our approach and ensure we are truly protecting those at risk.
Footnotes:
(1) Wellm, D.; Zentgraf, K. Diagnostic Tools for Return-to-Play Decisions in Sports-Related Concussion. J Concussion 2023, 7. https://doi.org/10.1177/20597002231183234.
(2) Giza, C. C.; Hovda, D. A. The New Neurometabolic Cascade of Concussion. Neurosurgery 2014, 75, S24–S33. https://doi.org/10.1227/NEU.0000000000000505.
(3) Hong, Y.; Boiti, A.; Vallone, D.; Foulkes, N. S. Reactive Oxygen Species Signaling and Oxidative Stress: Transcriptional Regulation and Evolution. Antioxidants. Multidisciplinary Digital Publishing Institute (MDPI) March 1, 2024. https://doi.org/10.3390/antiox13030312.