Did you know that Alzheimer’s disease (AD) might have more in common with diabetes than we ever imagined? Scientists have discovered a powerful link between insulin resistance – the same problem at the heart of Type 2 Diabetes – and the brain changes seen in Alzheimer’s. Some even call AD “Type 3 Diabetes” because of how insulin dysfunction contributes to memory loss and cognitive decline. But how does this work? And could diabetes medications help fight Alzheimers? [1]

Figure 1 [2]
Insulin: More Than Just a Blood Sugar Regulator
We usually think of insulin as the hormone that controls blood sugar, but it also plays a vital role in the brain. Insulin helps neurons communicate, protects them from damage, and keeps brain cells energized. When everything is working well, insulin binds to receptors on brain cells, triggering pathways that support learning and memory.
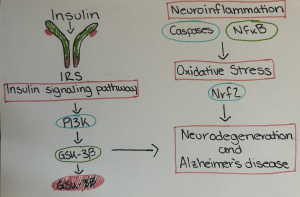
Figure 2 [3]: Artstract by Ella Alsleben. Diagram illustrating how insulin signaling through IRS, PI3K, and GSK3 beta interacts with neuroinflammation and oxidative stress pathways – via molecules like caspsases, NFkB, and Nrf2 – to contribute to neurodegeneration and Alzheimer’s disease.
But when insulin signaling is disrupted – known as brain insulin resistance – neurons can’t absorb glucose efficiently, leading to energy shortages, inflammation, and cell damage. This makes it harder for the brain to function, setting the stage for Alzheimer’s. [4]
The Early Warning Signs: Insulin Resistance in the Brain
Long before severe memory loss kicks in, brain insulin resistance begins to take hold – especially in areas critical for memory, like the hippocampus and cortex. Here’s what happens:
- Neurons stop responding to insulin: Key signaling pathways that keep brain cells alive and functioning begin to break down.
- Glucose metabolism slows down: Brain scans show that memory-related areas start using less glucose, making it harder to form new memories.
- Inflammation and oxidative stress rise: Harmful molecules like TNF-a and IL-6 flood the brain, damaging neurons and worsening insulin resistance.
Adding to the problem, amyloid-beta oligomers – toxic protein clumps linked to AD – can actually cause insulin resistance in neurons. This creates a vicious cycle: insulin dysfunction fuels Alzheimer’s, and Alzheimer’s worsens insulin resistance. [5]
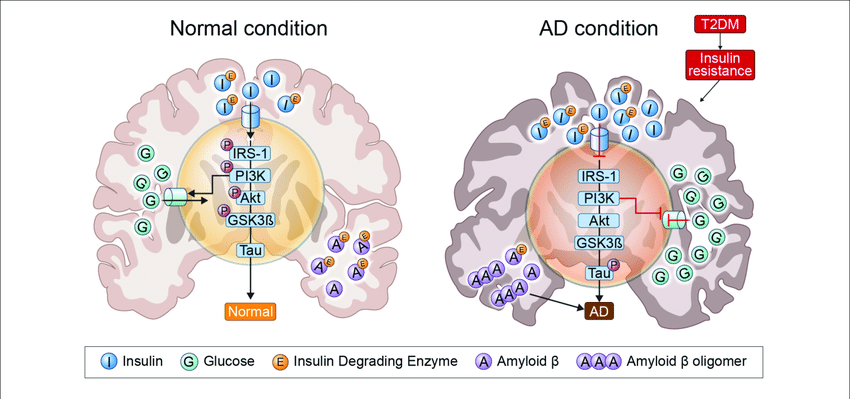
Figure 3 [6]
As Alzheimer’s Progresses: Insulin Dysfunction Gets Worse
As the disease advances, insulin resistance in the brain becomes severe:
- Insulin receptors break down: The brain can’t properly respond to insulin, leading to widespread metabolic failure.
- Neurons lose their survival signals: Key pathways, like P13K/Akt, that protect against cell death become disrupted.
- Brain cells starve: Glucose metabolism crashes, leaving neurons without the energy they need to survive.
- Amyloid plaques and tau tangles grow: These toxic proteins further block insulin signaling, accelerating brain cell death. [7]
Diabetes and Alzheimer’s: A Dangerous Connection
People with Type 2 Diabetes Mellitus (T2DM) are at a higher risk of developing Alzheimer’s – likely because both conditions involve insulin resistance and chronic inflammation. Research suggests that high insulin levels in the body can actually reduce insulin transport into the brain, making the problem worse.
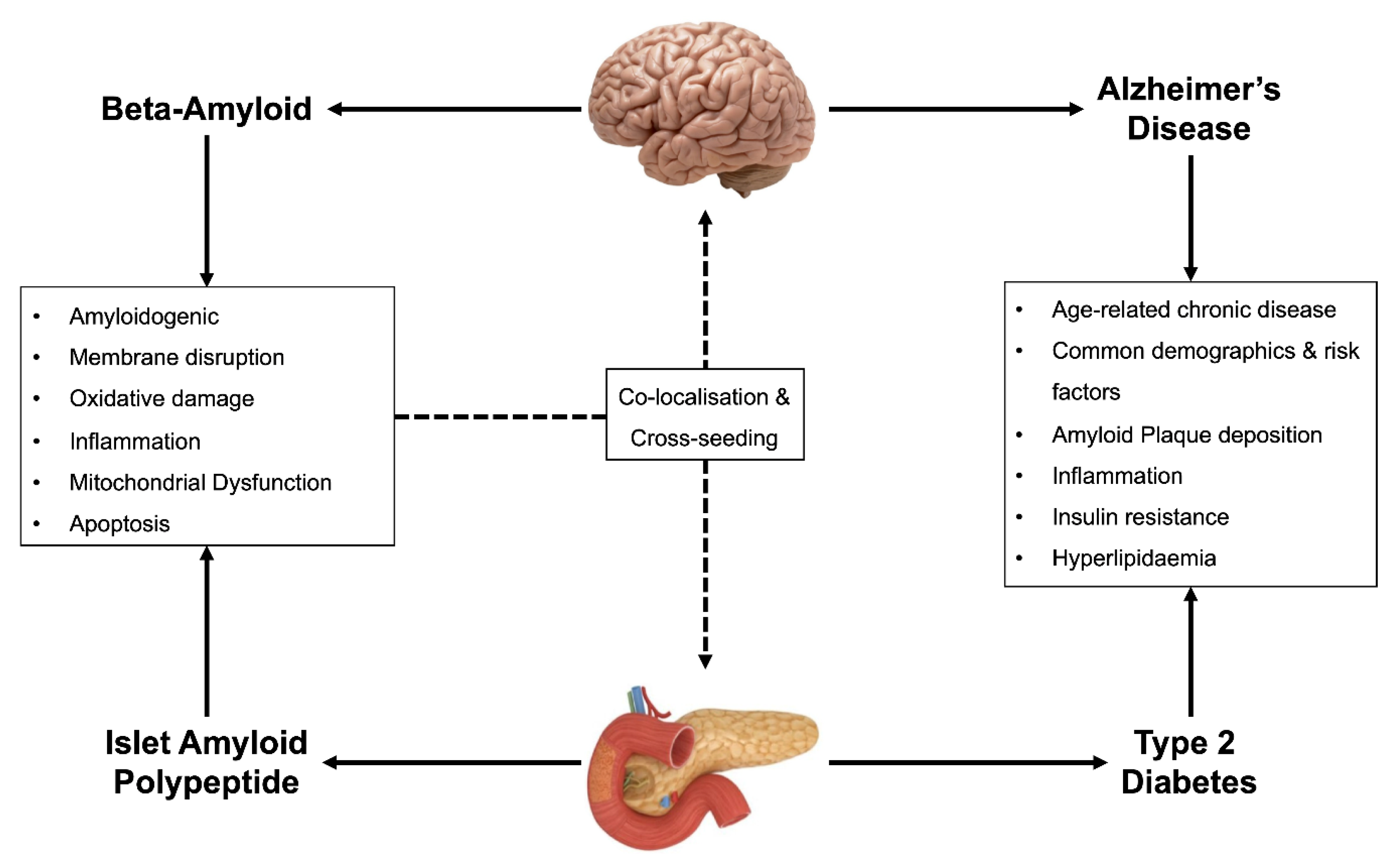
Figure 4 [8]
Can Diabetes Drugs Help Treat Alzheimer’s?
- Metformin: A common diabetes drug that may improve insulin sensitivity and reduce tau protein buildup in the brain.
- Intranasal Insulin: Direct delivery of insulin to the brain (through the nose) has shown improvements in memory and cognitive function.
- GLP-1 Receptor Agonists (e.g., Exenatide): These diabetes medications enhance insulin signaling and have anti-inflammatory effect in the brain.
- Thiazolidinediones (e.g., Pioglitazone): These drugs improve insulin sensitivity and may reduce amyloid plaque formation.
Final Thoughts: What Can You Do?
While research on insulin-based Alzheimer’s treatments is ongoing, one thing is clear: managing blood sugar and insulin levels is crucial for brain health.
Here are some lifestyle tips to help reduce your risk:
- Eat a balanced diet rich in Whole Foods, healthy fats, and fiber.
- Exercise regularly to improve insulin sensitivity.
- Get quality sleep – poor sleep can worsen insulin resistance.
- Manage stress, as chronic stress affects insulin function.

Figure 5 [9]
Alzheimer’s disease is still a mystery in many ways, but understanding the insulin connection opens up new treatment possibilities. As science continues to evolve, one thing remains certain: taking care of your metabolic health is one of the best things you can do for your brain!
References
[1] de la Monte, S. M., & Wands, J. R. (2008). Alzheimer’s disease is type 3 diabetes—evidence reviewed. Journal of Diabetes Science and Technology, 2(6), 1101–1113. https://doi.org/10.1177/193229680800200619
[2] Man measuring blood sugar pictures, images and stock photos. iStock. (n.d.). https://www.istockphoto.com/photos/man-measuring-blood-sugar
[3] Artstract by Ella Alsleben
[4]Akhtar, A., & Sah, S. P. (2020). Insulin signaling pathway and related molecules: Role in neurodegeneration and alzheimer’s disease. Neurochemistry International, 135, 104707. https://doi.org/10.1016/j.neuint.2020.104707
[5] Arnold, S. E., Arvanitakis, Z., Macauley-Rambach, S. L., Koenig, A. M., Wang, H.-Y., Ahima, R. S., Craft, S., Gandy, S., Buettner, C., Stoeckel, L. E., Holtzman, D. M., & Nathan, D. M. (2018). Brain insulin resistance in type 2 diabetes and alzheimer disease: Concepts and conundrums. Nature Reviews Neurology, 14(3), 168–181. https://doi.org/10.1038/nrneurol.2017.185
[6] Zimy. (2024, April 2). Insulin and alzheimer’s disease. Cobbers on the Brain. https://blog.cord.edu/cobbersonthebrain/2024/04/02/insulin-and-alzheimers-disease/
[7] Akhtar, A., & Sah, S. P. (2020). Insulin signaling pathway and related molecules: Role in neurodegeneration and alzheimer’s disease. Neurochemistry International, 135, 104707. https://doi.org/10.1016/j.neuint.2020.104707
[8] Movassat, J., Delangre, E., Liu, J., Gu, Y., & Janel, N. (2019, June 3). Hypothesis and theory: Circulating alzheimer’s-related biomarkers in type 2 diabetes. insight from the goto-kakizaki rat. Frontiers. https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2019.00649/full
[9] Sarkar, N. (n.d.). Embrace healthy lifestyle, take balanced diet, exercise, sleep, stress relief, no smoking. Vecteezy. https://www.vecteezy.com/vector-art/46149206-embrace-healthy-lifestyle-take-balanced-diet-exercise-sleep-stress-relief-no-smoking