Imagine your brain as a city, with neurons acting like workers who keep everything running smoothly. For these workers to do their job—helping you think, remember, and move—they need energy. Insulin, a hormone that helps control sugar levels, is like the key that unlocks fuel for these workers. But when something goes wrong with insulin, the whole city starts falling apart.
The Role of Insulin in Brain Health
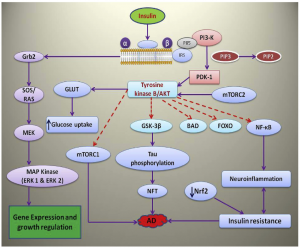
Insulin plays a crucial role in brain function, influencing memory, cognition, and overall neural health. In a healthy brain, insulin supports synaptic plasticity, enhances neuronal survival, and regulates energy metabolism. However, when insulin signaling is impaired, as seen in insulin resistance, it can contribute to neurodegeneration and cognitive decline.
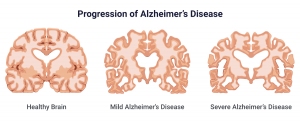
One of the major consequences of insulin resistance in the brain is its impact on the formation of neurofibrillary tangles (NFTs) and amyloid-beta (Aβ) plaques, two hallmarks of Alzheimer’s Disease (AD). Insulin resistance leads to increased oxidative stress and inflammation, which in turn activate kinases such as GSK-3β. This enzyme plays a central role in hyperphosphorylating tau proteins, leading to the formation of NFTs that disrupt neuronal communication and eventually cause cell death.
Additionally, insulin plays a role in regulating the clearance of Aβ peptides from the brain. Under normal conditions, insulin-degrading enzyme (IDE) helps break down Aβ, preventing it from accumulating. However, when insulin levels are chronically elevated due to insulin resistance, IDE becomes increasingly occupied with degrading insulin rather than Aβ. This imbalance leads to an accumulation of toxic Aβ plaques, further exacerbating neurodegeneration.
Moreover, insulin resistance can disrupt the function of GLUT4, a glucose transporter critical for neuronal energy metabolism. Impaired glucose uptake deprives neurons of essential energy, leading to synaptic dysfunction and cognitive impairment.
Studies have shown that insulin administration, either peripherally or intranasally, can enhance memory and cognitive function by improving glucose metabolism, reducing tau phosphorylation, and aiding in Aβ clearance. This suggests that therapies targeting insulin signaling pathways may hold promise in preventing or slowing the progression of AD.
Overall, maintaining insulin sensitivity through lifestyle interventions such as regular exercise, a balanced diet, and metabolic health optimization can significantly reduce the risk of AD and support overall brain function. [1]
 [1]
[1]
Why This Matters for Alzheimer’s, Parkinson’s, and Huntington’s
- Alzheimer’s Disease (AD):
- Insulin normally prevents the buildup of toxic proteins like amyloid plaques and tau tangles (which clog up brain cells like roadblocks in a city).
- Without insulin’s help, these roadblocks grow, leading to memory loss and cognitive decline.
- Parkinson’s Disease (PD):
- The brain region responsible for movement, the substantia nigra, depends on insulin to keep dopamine levels balanced.
- When insulin resistance occurs, dopamine-producing cells die, causing tremors, stiffness, and difficulty moving.
- Huntington’s Disease (HD):
- Insulin helps control energy production and repair damaged cells.
- In Huntington’s, insulin signaling is disrupted, leading to motor problems and brain cell degeneration.
The Role of Genetics in Alzheimer’s Disease
While lifestyle factors like diet and exercise play a big role in brain health, genetics can also increase the risk of developing AD. One of the biggest genetic risk factors is a gene called APOE (Apolipoprotein E), particularly the APOE4 variant.
- People with one copy of APOE4 have an increased risk of AD.
- Those with two copies (one from each parent) have an even higher risk and may develop symptoms earlier.
- On the other hand, people with the APOE2 variant seem to have a lower risk.
Other genes involved in brain inflammation, insulin signaling, and tau protein regulation also play a role, but having a high-risk gene does not mean someone will definitely get AD. It just means they need to be extra careful with lifestyle choices to reduce their risk. [2]
Reducing the Risk of Alzheimer’s
Even if someone has a genetic risk for AD, behavioral changes can significantly lower the chances of developing the disease. Research suggests the following as ways of reducing the risk of Alzheimer’s:
- Keep Blood Sugar and Insulin in Check
- Avoid processed foods, sugary drinks, and excessive refined carbs, as they contribute to insulin resistance.
- Eat a Mediterranean or low-carb diet, rich in healthy fats (olive oil, nuts, fish) and antioxidants. [3]
- Stay Physically Active
- Exercise increases insulin sensitivity, reduces inflammation, and boosts brain-derived neurotrophic factor (BDNF), which helps grow new brain cells.
- Aim for at least 150 minutes of moderate exercise per week (walking, swimming, or strength training).
- Improve Sleep Quality
- Sleep removes toxins from the brain, including harmful amyloid proteins linked to AD.
- Stick to a consistent sleep schedule and avoid screens before bedtime.
- Reduce Stress and Inflammation
- Chronic stress increases cortisol, which contributes to brain damage.
- Practice meditation, yoga, or deep breathing to reduce stress hormones.
- Stay Mentally and Socially Active
- Challenge your brain with reading, puzzles, or learning a new skill.
- Social engagement reduces inflammation and keeps the brain stimulated. [4]
- Consider Fasting or Time-Restricted Eating
- Intermittent fasting or time-restricted eating (12-16 hours of fasting overnight) helps regulate insulin and may support brain function. [3]
It should be noted that these are all examples of things that every person should try to aim for to remain healthy. However, this is not an exhaustive list and it is also important that we do not stress over the mere possibility of becoming sick with a disease so much that we cannot live our lives.
 [5]
[5]
Can Insulin Be a Solution?
The good news is that boosting insulin sensitivity—either through medications, lifestyle changes, or natural compounds—could slow down or even prevent these diseases. Exercise, a healthy diet, and certain drugs that activate the Nrf2 pathway or insulin receptors could help protect brain cells, reduce inflammation, and restore lost function. [1]
Final Thoughts
Your brain and body are deeply connected, and problems like insulin resistance and inflammation don’t just lead to diabetes—they may also be the missing link behind memory loss and neurodegenerative diseases. The more we understand about how insulin works in the brain, the closer we get to finding new treatments for Alzheimer’s, Parkinson’s, and other brain disorders.
To read more about the specifics about Alzheimer’s disease and insulin resistance click here.
[1]
- Akhtar and S. P. Sah, “Insulin signaling pathway and related molecules: Role in neurodegeneration and Alzheimer’s disease,” Neurochemistry International, vol. 135, p. 104707, May 2020, doi: 10.1016/j.neuint.2020.104707.
[2]
- Safieh, A. D. Korczyn, and D. M. Michaelson, “ApoE4: an emerging therapeutic target for Alzheimer’s disease,” BMC Med, vol. 17, no. 1, p. 64, Dec. 2019, doi: 10.1186/s12916-019-1299-4.
[3]
What do we know about diet and prevention of alzheimer’s disease? | National Institute on Aging, https://www.nia.nih.gov/health/alzheimers-and-dementia/what-do-we-know-about-diet-and-prevention-alzheimers-disease (accessed Feb. 2025).
[4]
Preventing alzheimer’s disease: What do we know? | National Institute on Aging, https://www.nia.nih.gov/health/alzheimers-and-dementia/preventing-alzheimers-disease-what-do-we-know (accessed Feb. 2025).
[5]
“Alzheimer’s disease: Causes, stages, Symptoms & Prevention,” Drugwatch.com, https://www.drugwatch.com/health/alzheimers-disease/ (accessed Feb. 2025).