For decades, we’ve pointed fingers at willpower and calories in the battle against obesity. Eat less. Move more. Sounds simple, right?
But what if we’ve been missing a critical piece of the puzzle all along – something hidden deep within the brain? What if, instead of a lack of self-control, the true culprit behind rising obesity rates is inflammation in the brain itself?
A Crisis Hiding in Plain Sight
Obesity is no longer just a personal health concern – it’s a global epidemic. Despite the flood of diet plan, exercise apps, and miracle weight-loss pills, the numbers keep climbing. And while conventional wisdom tells us it’s all about lifestyle choices, a growing body of research is challenging that narrative.
One groundbreaking shift in our understanding comes from the field of neuroscience, where researchers have begun investigating how inflammation in the brain – specifically, in a region called the hypothalamus – might be silently sabotaging our efforts to maintain a healthy weight. [1]
Meet Your Brain’s Control Center
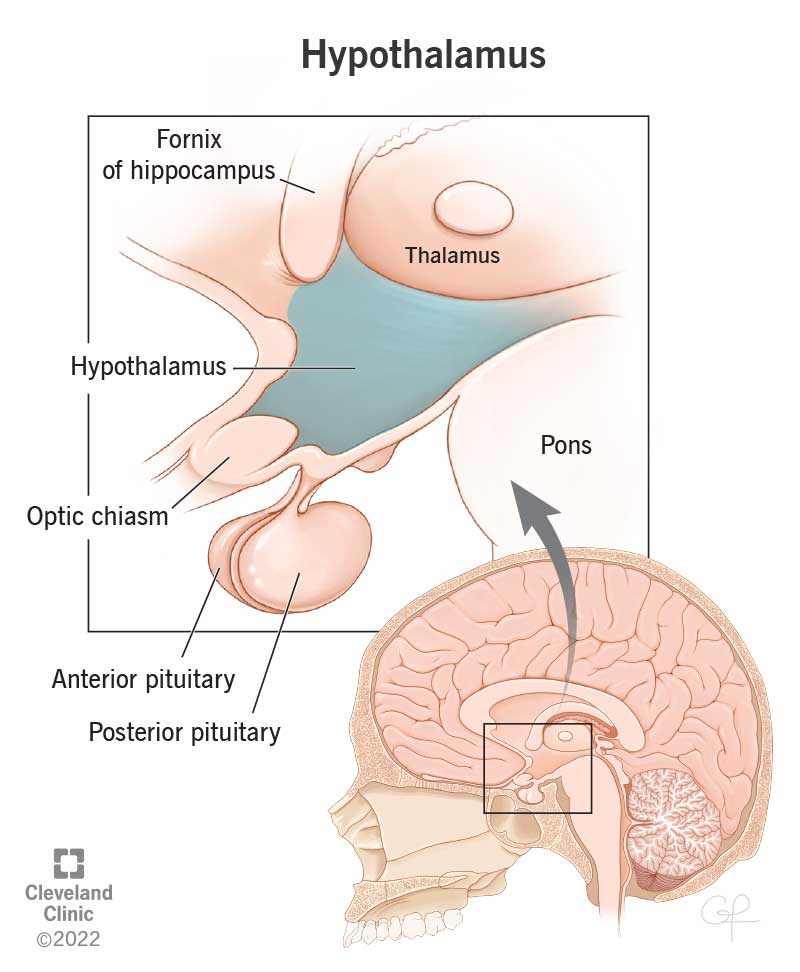
Think of the hypothalamus as your body’s internal thermostat for energy (Figure 1). This small but mighty structure regulates hunger, satiety (that feeling of fullness), body temperature, and metabolism. It’s constantly receiving signals from hormones like leptin and insulin, helping the body make smart decisions about when to eat and when to stop. But when this delicate system in thrown off by chronic inflammation, the entire process goes haywire. [2]
Figure 1 [3] The hypothalamus helps manage your body temperature, hunger and thirst, mood, sex drive, blood pressure and sleep.
The Hidden Fire Within
Recent studies, like the one reviewed by researchers Jais and Burning, have illuminated how brain inflammation may play a far more active role in obesity than we ever imagined. Here’s what the science reveals:
- It starts sooner than you think: Within just days of switching to a high-fat diet, signs of inflammation begin to appear in the hypothalamus. This inflammation doesn’t wait for the number on the scale to climb – it often precedes noticeable weight gain. In other words, the damage may begin before you even realize anything is wrong. [1]
- Brain cells join the battle: Under normal conditions, cells in the brain known as microglia and astrocytes act as its maintenance crew, keeping things clean and running smoothly. But when exposed to excess dietary fat, these cells go into overdrive. They start pumping out inflammatory molecules like TNF-alpha and IL-6, which begin to damage the neurons responsible for hunger and metabolism regulation (Figure 2). [1]
- Hormonal static: As inflammation ramps up, your hypothalamus starts to lose its ability to respond to leptin and insulin – two critical hormones that tell your brain, “We’ve got enough energy; we don’t need more food.” With this signaling broken, the brain keeps shouting for food, even when the body is full. The result? A cycle of overeating, insulin resistance, and further weight gain (Figure 2). [1]
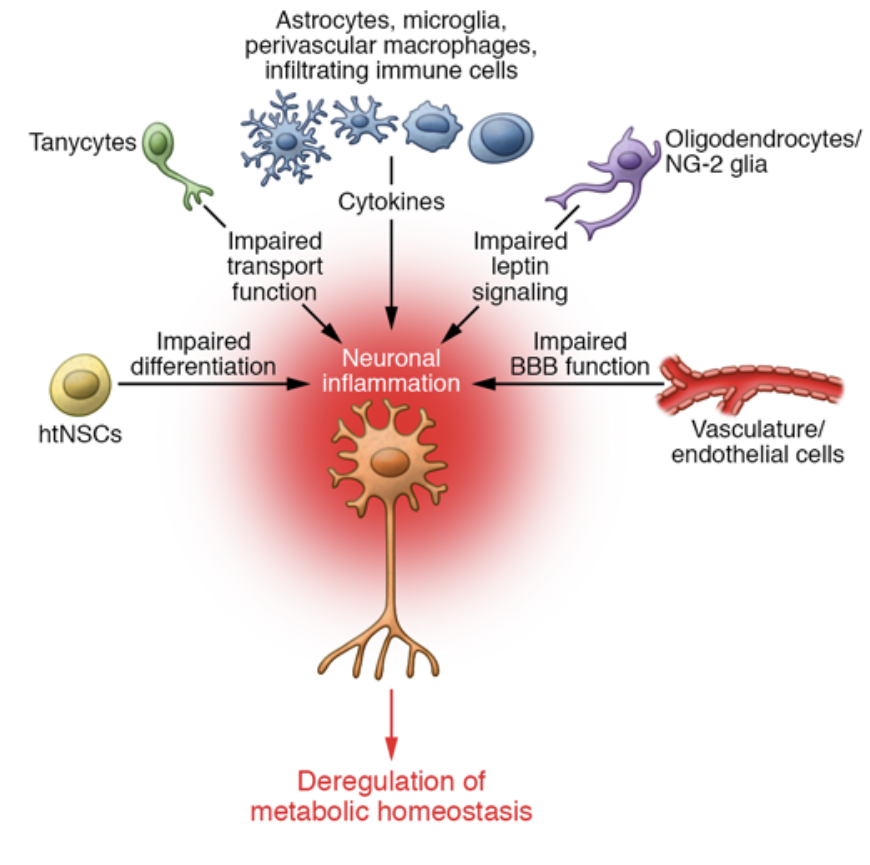
Figure 2 [1] Cellular network of hypothalamic inflammation.
Why This Matters (More Than You Might Think)
This isn’t just fascinating science – it’s deeply personal. Millions of people struggle with their weight despite eating well, exercising regularly, and following medical advice. And when the pounds don’t budge, the default explanation is often self-blame.
But what if the issue isn’t a lack of effort – but an inflamed brain working against you?
Understanding the role of hypothalamic inflammation reframes the entire conversation. It removes the stigma and shame so often attached to obesity and offers a new lens: what if your Brian is just trying to protect you, but got its are crossed along the way?
Need some further explanation? Watch this video by Yuri Elkaim:
A New Path Forward
The good news is that this research doesn’t just point out a problem – it also lights the way to potential solutions. Scientists are now exploring treatments aimed at reducing inflammation in the brain as a way to restore proper metabolic function. [1]
Early animal studies show that compounds like IL-10 agonists – which help cool down brain inflammation – could reverse some of the hypothalamic damage, improve insulin sensitivity, and even normalize appetite signals. It’s still early days, but the implications are enormous. [4]
Hope on the Horizon
There’s still so much we don’t understand about the intricate dance between brain, body, and metabolism. But one thing is becoming clear: the old narrative about willpower and laziness no longer holds up.
Obesity isn’t just a simple math problem of calories in and out. It’s a complex neurobiological condition, influenced by inflammation, hormones, and brain function (Figure 3). And by looking deeper – literally, into the brain – we can start to craft smarter, more compassionate solutions. [1]
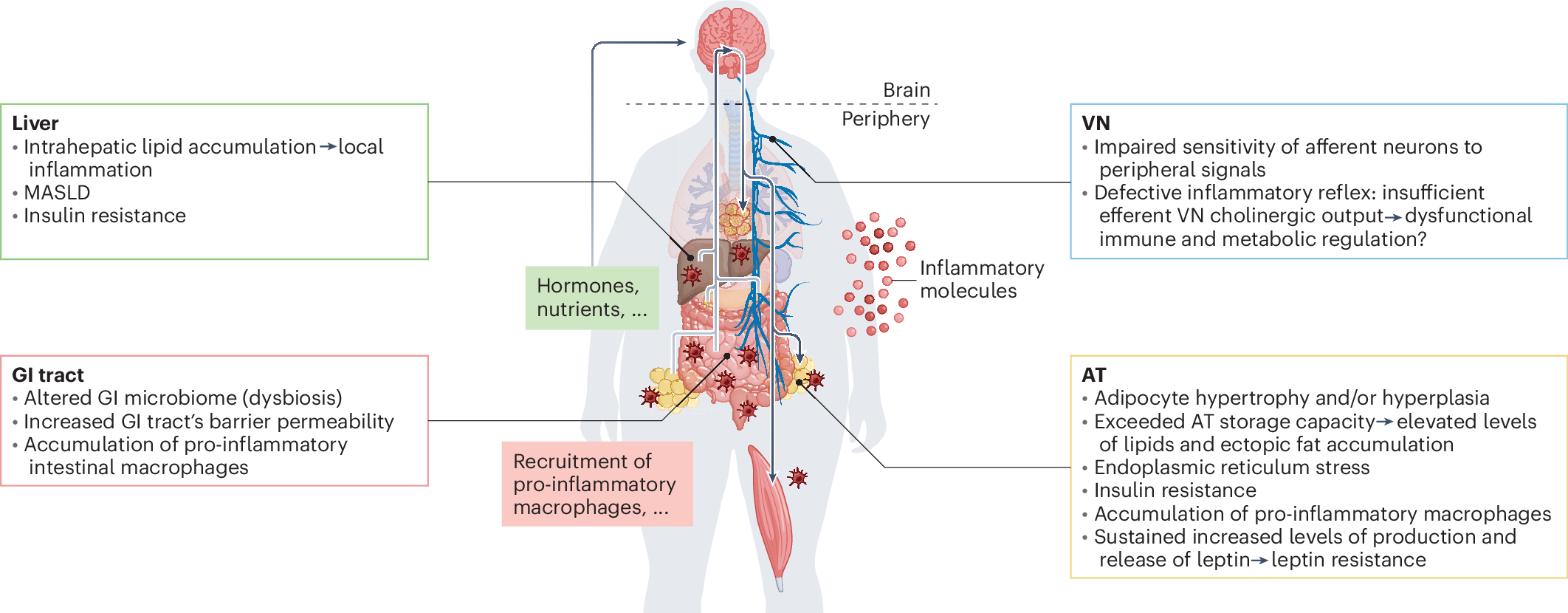
Figure 3 [5] Illustrates how chronic inflammation affects multiple organs, disrupting hormone signaling, immune responses, and metabolism, which collectively contribute to obesity and metabolic disease.
So the next times someone tells you “just eat less and exercise more,” remember this…the real fight might not be in your fridge or at the gym… it might be happening deep inside your brain.
References
[1] Jais, A., & Brüning, J. C. (2017). Hypothalamic inflammation in obesity and metabolic disease. Journal of Clinical Investigation, 127(1), 24–32. https://doi.org/10.1172/jci88878
[2] Yeung, A. Y. (2023, January 3). Physiology, obesity neurohormonal appetite and Satiety Control. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK555906/
[3] professional, C. C. medical. (2025, March 3). Hypothalamus: What it is, function, conditions & disorders. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22566-hypothalamus
[4] Ropelle ER, et al. IL-6and IL-10 anti-inflammatory activity links exercise to hypothalamic insulin and septic sensitivity through IKKbeta and ER stress inhibition. PLoS Biol. 2010;8(8):e1000465.
[5] Le Thuc, O., & García-Cáceres, C. (2024, July 12). Obesity-induced inflammation: Connecting the periphery to the brain. Nature News. https://www.nature.com/articles/s42255-024-01079-8