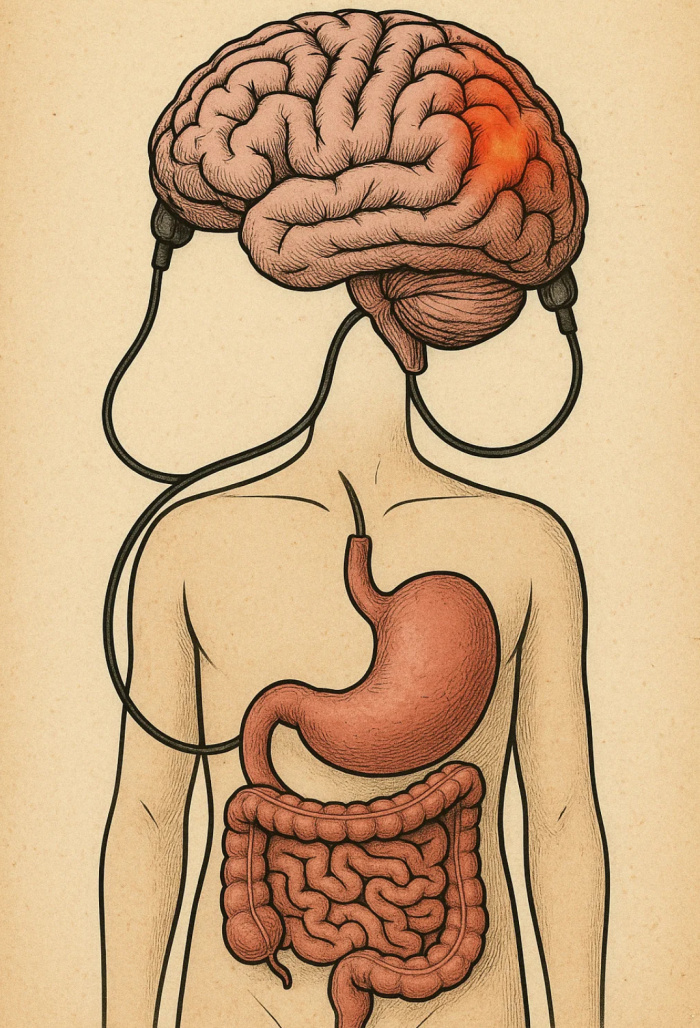
Abstract by Alisha Debleye: This depicts the connection of the Gut and the inflammation on the brain.
Let me take you on a journey that begins not in a fast food drive-thru or a grocery aisle stocked with ultra processed snacks, but inside the brain, in a small yet powerful region called the hypothalamus. It’s a place where every bite we take and every calorie we burn is carefully regulated by complex signaling systems. This tiny structure is the conductor of our body’s energy orchestra.
And for most of human history, this system worked just fine. We ate what we needed, our hormones sent signals to stop eating, and our bodies used energy efficiently. But in today’s world, with diets high in saturated fats and sugar, this ancient system is under attack. What starts on our plates ends up disrupting our brains, literally inflaming them. Therefore, obesity is no longer just a “weight issue.” It’s a neurological condition with deep consequences for public health in the United States.
A Silent Fire in the Brain
A groundbreaking study published in the Journal of Clinical Investigation reveals that obesity-related inflammation begins not in the belly or the thighs, but in the hypothalamus, the very part of the brain that regulates hunger and energy use1.
Within just three days of starting a high-fat diet, inflammation begins to flare in this region. Before any weight is visibly gained, the hypothalamus starts to lose sensitivity to insulin and leptin, two hormones responsible for telling us when to stop eating1. As this feedback loop breaks down, overeating begins.

Figure 1: In healthy brains, leptin and insulin suppress appetite through neurons in the arcuate nucleus (ARC). But in inflamed brains, this signal is ignored, fueling increased hunger and weight gain.
The Domino Effect
As hypothalamic inflammation sets in, it doesn’t stay put. Microglia, the brain’s immune cells, begin releasing inflammatory molecules like TNF-α and IL-6. These cytokines damage nearby neurons and spread dysfunction throughout the brain. The blood-brain barrier becomes more permeable, allowing even more inflammatory substances to enter.
The science is clear. Diet-induced inflammation impairs our ability to feel full and use energy properly, leading to a vicious cycle of overeating and weight gain1.
And the damage isn’t limited to neurons. Astrocytes, another type of brain cell, swell and become reactive. Their once-helpful support turns toxic, and they start producing molecules that accelerate the inflammatory cascade. Over time, this neural chaos disrupts synaptic communication and even leads to neuron death, especially in the ARC region, which governs satiety.
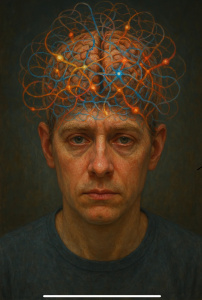
Abstract by Alisha Debleye: Depicting the connections around the brain and how each part is a domino effect when things go wrong.
The Price We Pay
This is more than just a scientific curiosity. It’s a national crisis. In the U.S., more than 42% of adults are obese, and the medical costs are staggering, an estimated $147 billion per year2.
And yet, so much of the public conversation around obesity is still framed as a moral failing, a lack of willpower. The truth is, chronic exposure to high-fat, high-sugar diets rewires our brains, making it biologically harder to stop eating.
Worse yet, this inflammation may start even before birth. Research shows that maternal obesity primes the developing brains of offspring for inflammation, setting them up for metabolic disorders later in life1.
Hope in Reversal
But here’s where it gets hopeful.
Studies suggest that unsaturated fats, particularly omega-3 fatty acids, can reverse some of this hypothalamic inflammation1. Exercise, too, has been shown to reduce cytokine activity in the brain, restoring insulin and leptin sensitivity. And promising new therapies target the inflammatory pathways directly, from NF-κB inhibitors to drugs that reduce endoplasmic reticulum (ER) stress.
In other words, early intervention matters. The fire in the brain can be extinguished if we act fast enough.
Why This Matters to You
This isn’t just another health scare story. It’s a wake-up call.
We need to rethink how we talk about, and treat, obesity. We need public policies that address the quality of our food supply, not just calorie counts. We need compassion, not blame. And we need research funding that prioritizes neurological and inflammatory causes of obesity.
If the brain controls the body, then protecting the brain should be the first line of defense in tackling the obesity epidemic.
So next time you hear someone say, “Just eat less,” remember: it’s not always that simple. Behind every craving, every binge, and every struggle with weight may be a brain under siege.
Let’s stop judging. Let’s start understanding. Let’s cool the fire, one neuron at a time.
References:
[1] Jais, A., & Brüning, J. C. (2017). Hypothalamic inflammation in obesity and metabolic disease. *The Journal of Clinical Investigation*, 127(1), 24–32. https://www.jci.org/articles/view/88878
[2] CDC. (2022). Adult Obesity Facts. https://www.cdc.gov/obesity/data/adult.html
