We’ve all seen the movie villain who always seems one step ahead—dodging every trap, escaping every jail cell, and outsmarting the hero. That’s kind of what it feels like trying to treat mesenchymal glioblastoma (GBM)—a sneaky, aggressive form of brain cancer that plays by its own rules.
GBM, or glioblastoma, is already one of the deadliest brain tumors. It grows fast and spreads like wildfire, and despite surgery, radiation, and chemo, most people diagnosed with it only live about 14 months. Doctors and researchers are doing everything they can to fight back…
But mesenchymal GBM is particularly hard to beat.
This subtype isn’t just another face in the crowd. It’s the troublemaker of the GBM family. While all GBM tumors are aggressive, mesenchymal GBM comes with its own toolkit of genetic mutations that make it especially nasty. It mutates tumor suppressor genes like NF1 and PTEN, which normally help control cell growth and death. Without them, cancer cells have free rein to survive, grow, and invade healthy brain tissue like an evil army on a mission.
Imagine trying to shut down a building’s power supply to stop a rogue machine—but finding out there’s a secret generator in the basement. That’s what it’s like targeting mesenchymal GBM: every time we try to block one growth signal, another pathway kicks in and keeps the tumor going.
Therefore, scientists are rethinking how they approach this villain.
Instead of chasing each pathway one by one (like trying to plug leaks in a sinking ship), researchers are looking for the convergence points—places where multiple signaling pathways come together. Think of it like cutting off a criminal’s access to both their car and their getaway plane in one move.
The Science Behind the Scene
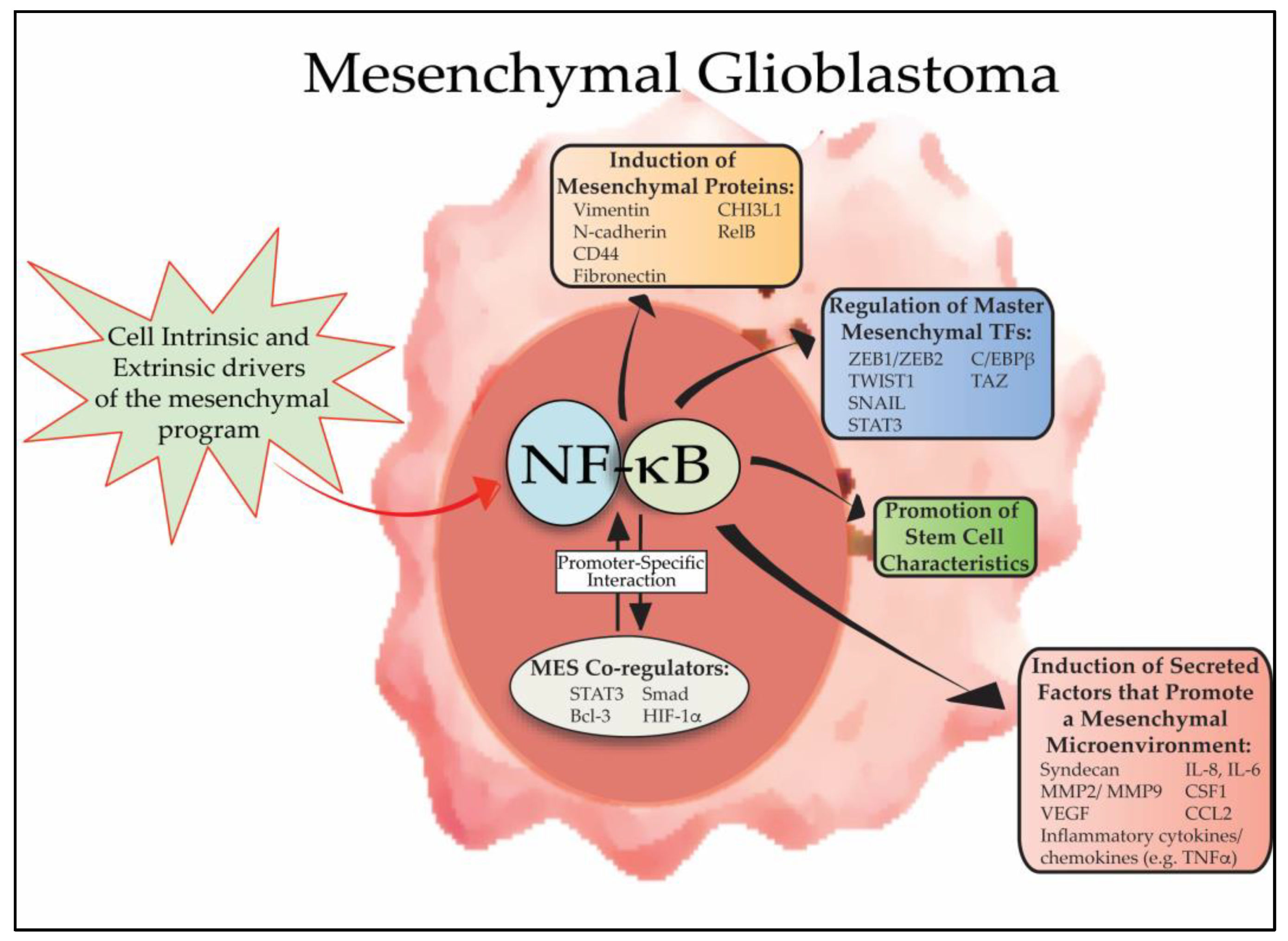
Researchers have also found that mesenchymal GBM tricks the immune system by turning up a protein called PD-L1. This protein acts like an invisibility cloak, stopping immune cells from attacking. So now, doctors are testing new therapies that combine pathway blockers and immunotherapy—like a tag team effort to remove the cloak and cut off the tumor’s power at the same time. It’s complex stuff, but here’s the hope: by understanding how this cancer cheats the system, we can finally beat it at its own game.
The Problem With One-Lane Therapies
Doctors have tried targeting these pathways before, but here’s the kicker: mesenchymal GBM is really good at adapting. You block one road, it takes a detour. You hit it with chemo, it uses backup routes. This is why many treatments work for a little while, but then the tumor comes back—stronger.
But researchers are now realizing that maybe we’ve been looking at this all wrong. Instead of trying to shut down each road one by one, what if we focused on where all the roads merge?
That’s where a protein called CREB comes in. Think of CREB as a command center—a place where multiple signals from different pathways arrive and trigger cancer-promoting genes. CREB helps GBM cells survive, grow, invade the brain, and even evade the immune system [3].
By targeting CREB, we don’t just block one route—we potentially block them all. That’s the kind of big-picture thinking this cancer demands.
So, Now What’s Next?

Researchers are testing new combinations of therapies. Some aim to shut down MAPK and PI3K at the same time. Others are experimenting with boosting a lesser-known pathway—cAMP, which usually acts as a tumor suppressor in GBM. The most exciting idea? Going after CREB, the “hub,” instead of the “spokes.”
Therefore, mesenchymal GBM is teaching us that to defeat a shape-shifting cancer, we need shape-shifting strategies—ones that understand how cancer talks to itself, adapts, and survives. The science isn’t just fascinating—it’s offering hope.
This isn’t just about brain cancer—it’s about how we think. Mesenchymal GBM is showing us that the best way to solve complex problems isn’t brute force, it’s systems thinking. Whether you’re battling a disease, launching a startup, or just trying to figure out life, the same rule applies:
Zoom out. Find the patterns. Target the center.
Resources
[1] Yamini, B. (2018). NF-κB, Mesenchymal Differentiation and Glioblastoma. Cells, 7(9), 125. https://doi.org/10.3390/cells7090125
[2] Fung, N. H., Grima, C. A., Widodo, S. S., Kaye, A. H., Whitehead, C. A., Stylli, S. S., & Mantamadiotis, T. (2019). Understanding and exploiting cell signalling convergence nodes and pathway cross-talk in malignant brain cancer. Cellular Signalling, 57, 2–9. https://doi.org/10.1016/j.cellsig.2019.01.011
[3] Kim, H.-J., Jeon, H.-M., Batara, D. C., Lee, S., Lee, S. J., Yin, J., Park, S.-I., Park, M., Seo, J. B., Hwang, J., Oh, Y. J., Suh, S.-S., & Kim, S.-H. (2024). CREB5 promotes the proliferation and self-renewal ability of glioma stem cells. Cell Death Discovery, 10(1). https://doi.org/10.1038/s41420-024-01873-z
[4] Nowak, B., Rogujski, P., Janowski, M., Lukomska, B., & Andrzejewska, A. (2021). Mesenchymal stem cells in glioblastoma therapy and progression: How one cell does it all. Biochimica et Biophysica Acta (BBA) – Reviews on Cancer, 1876(1), 188582. https://doi.org/10.1016/j.bbcan.2021.188582