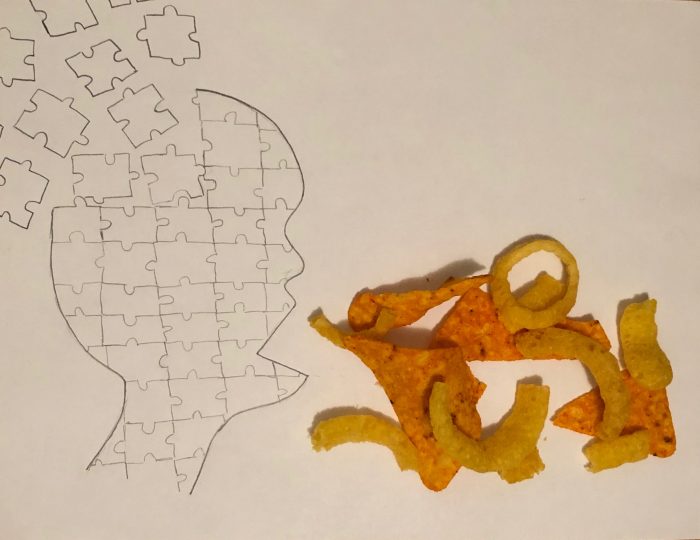
Did you know that 70% of people with type II diabetes are later diagnosed with Alzheimer’s? That is a ridiculous percentage to be coincidental, but what could these two diseases possibly have in common? Well, recent studies have linked both diabetes and Alzheimer’s to unhealthy diets high in fats and sugar. These unbalanced diets can then lead to detrimental factors such as insulin resistance, the degradation of your blood-brain barrier, and inflammation. Let’s take a closer look at how your diet can affect these three ailments.
Insulin Resistance:
Insulin is a natural hormone produced in the body when blood glucose levels are too high. It signals for the uptake and storage of glucose from the bloodstream to cells on the brain, liver, muscles etc. It is a very important biological function that can be disrupted if too many gangliosides (specifically GM3) have been incorporated into one’s diet. Glycosides are modified lipids that are found inside cell membranes and play an important role in cell signaling and communication. Unfortunately, if there becomes an abundance of GM3s in the membrane, they can disrupt insulin signaling by separating insulin receptors from their secondary proteins. This halts the signaling cascade and prevents the cell from intaking excess glucose resulting in insulin resistance. Excess GM3s also play a crucial role in the feedback production of amyloid beta (Ab) peptides. Once GM3 is degraded into GD3, it signals for more Ab peptides to be produced into the extracellular matrix (ECM). Therefore if there is a continuous integration of new GM3 into our membranes, the concentration of GD3s will rise leading to an increase of Ab peptides in the ECM. This can then lead to aggregation of these peptides which results in Ab plaque formation which is a classic trademark of Alzheimer’s.
Blood Brain Barrier and Chronic inflammation:
Another important factor in both Diabetes and Alzheimer’s is chronic inflammation that causes irreversible cell damage over time. The million dollar question is what causes the inflammation? Some research has pointed to clues within the gut-brain-axis which is a model showing how the gut can affect brain function. Simply the gut-brain-axis states that toxins, molecules, or anything else we digest can more easily get into our bloodstream if our gut’s microbiota is out of whack. This then can lead to extreme problems if our blood brain barrier (bbb) is damaged letting dangerous chemicals enter into our brains and cause inflammation. Microbiota imbalance can be caused by numerous factors including genetics and our daily diet. A diet high in fat, sugar, and sodium can also lead to fat accumulation which has also been shown to degrade our bbb. Without the protective covering of astrocytes around our blood vessels, which make up the bbb, the foreign molecules are free to wreak havoc on our brains. The inflammation response then hyper-activates the processing of Ab Proteins placing a higher concentration of Ab peptides in the ECM. With a higher concentration of Ab peptides, comes plaque formation and eventual neuronal death causing impairment in brain function and Alzheimer’s.
Besides the accumulation of plaques, Ab peptides trigger the production of cytokines which are the signaling molecules for inflammation creating a vicious cycle. If we could one day stop the cycle of inflammation in the brain before serious damage has occurred then we could theoretically treat Alzheimer’s. Other interesting fields of study could include bbb repair, fixing the gut microbiota in Alzheimer’s patients, and the degradation of excess Ab peptides.
However, for now, the biggest preventative strategy for Alzheimer’s and type II diabetes is a healthy lifestyle and diet. What we put into our body’s today will come back to affect our quality of life in the future.
