
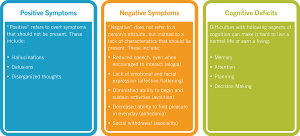
Schizophrenia is arguably one of the most difficult neurological diseases to understand if you do not have experience with it. Some of the symptoms are foreign and often frightening to a person. Putting yourself in the shoes of a someone who suffers from Schizophrenia is virtually impossible because of these symptoms. I will try to break down this diseases into understandable concepts that may give you some insight into the brain of a person with Schizophrenia. To begin, some symptoms make look like this:
- Delusions: Having constant thoughts that someone is out to get you or that a loved one is or is not really there; often follows logical reasoning but begins with the certainty that false thought is correct.
- Disorganized speech/behavior: Often trying to communicate their thoughts through nonsensical language; can get frustrated because they may be aware that their thoughts are not being communicated properly; disorganized behavior can look like continuous gestures with hands or body unknowingly.
- Hallucinations: These can include auditory and visual additions of perceptions that aren’t actually there; one may turn around and see a man with a knife, for example.
- Negative symptoms: Depressive symptoms are common in people with schizophrenia because of their different way of expressing emotions; often described as a feeling of being in a ‘mental fog’.
Moving on from symptoms, many people inside and out of the psychological field may brush Schizophrenia off as an “out there” disease because of the lack of knowledge of it’s cause and path in the brain. Schizophrenia is one of the most multi-faceted mental diseases, therefore making it extremely difficult to study. Here is what we do know:
- Schizophrenia is a chronic condition. Once diagnosed, you have it for life.
- There is no one cause of Schizophrenia. Rather, there are risk factors and hypotheses on what can be causes. These include:
- Genetic traits (often runs in families)
- Prenatal risk factors such as exposure to viruses and malnutrition
- Increased immune system activation (such as having an autoimmune disease)
- Childhood trauma
- Imbalances of neurotransmitters such as dopamine and glutamate in the brain
These risk factors are not very conclusive, but have given scientists and psychologists alike something to investigate. Recently, scientists have looked at the signaling pathways in the brain, what irregularities there are, and what treatment is doing for those irregular pathways.
Another issue that surrounds schizophrenia is the stigma that the disease carries with it. Schizophrenia is often thought of as the mental illness where patients just talk to themselves, are inappropriate or dangerous in public, or just seem crazy. These stereotypes do not help normalize this disease that effects about 1 in every 100 people. We wonder what would happen if Schizophrenia was treated like depression or anxiety is; how would that change the stigma? I would highly encourage you to watch this Ted Talk given by a professor who is diagnosed with Schizophrenia. She discusses her instances of psychosis as well as treatment, perseverance, and more.
To conclude, Samuel Keith, MD, editor of the America Journal of Psychiatry, describes Schizophrenia below:
“Real people with real feelings get schizophrenia. One should never underestimate the depth of their pain, even though the illness itself may diminish their ability to convey it….As one of my own patients told me, ‘Whatever this is that I have, I feel like I’m a caterpillar in a cocoon, and I’m never going to get the chance to be a butterfly.’”
https://www.verywellmind.com/the-internal-experience-of-schizophrenia-2953095
https://www.nimh.nih.gov/health/topics/schizophrenia/index.shtml