Amyotrophic lateral sclerosis (ALS) or Lou Gehrig’s disease, is the loss of motor neurons in the brain which leads to a gradual loss in muscle control. The early symptoms of ALS vary but can include: a loss of dexterity in hands or fingers, tripping or stumbling more frequently than normal, changes to one’s voice, or facial muscle spasms with inappropriate laughing or crying. Once diagnosed, the function in one’s extremities and skeletal muscle will continue to deteriorate until complete paralysis. Most people with ALS die from respiratory failure within two to five years after diagnosis.

The most horrific part about ALS is that the person’s brain remains unaffected meaning that they are completely conscious of their deterioration even in the very late stages of the disease. This is especially hard for end of life cares when the affected individual no longer has the ability to communicate to their caregivers. The fascinating part about this disease is the fact that average onset occurs between the ages of 40 and 70 years old. Scientists are trying to uncover what factors change in the brain to cause the drastic deterioration of only motor neurons. While research still has a long way to go, they have identified some key components to ALS and how they can cause such devastating symptoms.

There are two heavily supported hypotheses for the science behind ALS. One emphasizes oxidative stress while the other highlights RNA dysmetabolism. Recent studies have been trying to combine these two theories with the dilemma of finding out which one comes first. Right now, we know that gene mutations in SOD1 and FUS result in a decreased protection from reactive oxygen species (ROS). ROS are dangerous chemicals that can disrupt cell function and eventually lead to cell death. Besides losing the original function of these genes, these mutations make the proteins easier to aggregate and clump together. The accumulation of non-functional proteins can then severely impair cell function and also lead to cell death. The million dollar question is why do these events only occur in motor neurons and not in other cells of the brain? Unfortunately, we do not know which means as of right now we do not have a cure for ALS.
Figure 1. Shows the many affects protein aggregation can have on a cell’s function.
With no cures, doctors can only focus on treating the symptoms of the disease. However, with ALS there are minimal options for the alleviation of symptoms except for pain tolerance. This leads to the daily regimen of opioids with a continual increase in dosage as patients become tolerant. Because of these increasing doses, many ALS patients actually die from morphine overdoses instead of natural causes. As bad as it seems, what other options do patients have to die painlessly? Currently, only 7 states offer physician-assisted suicide which gives patients the right to end their lives if they have been diagnosed with a terminal illness and have a life expectancy of 6 months or shorter.
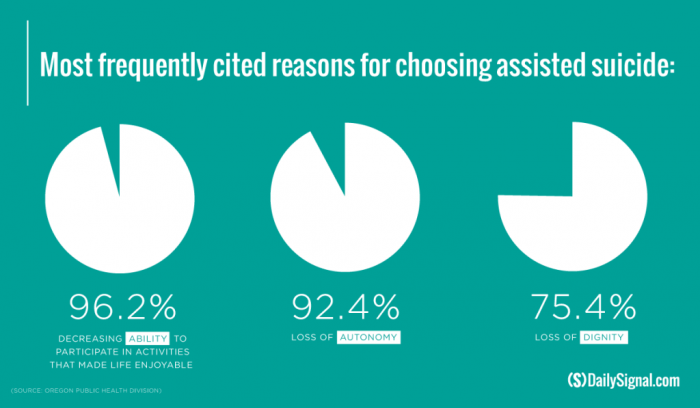
While end of life decisions can be uncomfortable, they need to be discussed thoroughly and brought to the attention of every state government. Right now, what is the difference between physician-assisted suicide and the universal right to refuse lifesaving treatment such as CPR, chemotherapy, or blood transfusions? Also, Healthcare professions always emphasis that patients have the right to die with dignity, but what dignity does one have when their only wish was to die before the pain and torment of a disease like ALS. Honest discussions must be made to further our understanding and acceptance of such end of life options that many countries like Canada, Germany, and Finland have already legalized.
