What’s the story?
Over the past decade, sugar has become an increasingly hot topic as a part of our diets. Updated recommendations have been in the news as recent as two days ago, which you can check out here.
Various cities and states have implemented (or tried to implement) sugary drink taxes to try and curb their populations’ never ending enthusiasm for these addictive sugar-laden foods. Many of the consequences of very high sugar intake are well known, like weight gain and type II diabetes. However, what a lot of people don’t know is how tightly linked diabetes and the development of Alzheimer’s are.
However, what a lot of people don’t know is how tightly linked diabetes and the development of Alzheimer’s are.
According to Mayo Clinic, a variety of studies have linked Alzheimer’s disease with diabetes, especially type two diabetes. While some studies are inconclusive and the mechanisms are poorly understood, there is certainly some connection between insulin signaling in the brain and the development of Alzheimer’s disease. In fact, many people with diabetes have changes in the brain that are indicative of both Alzheimer’s disease and vascular dementia. This may also contribute to the symptoms being seen, separate from an Alzheimer’s diagnosis. If you want to read more, here’s the article.
What’s the science?
First, here is a video giving a great visual overview of two of the most important processes going on in the brain during Alzheimer’s disease onset and progression, in addition to the variety of factors that also contribute to disease severity.
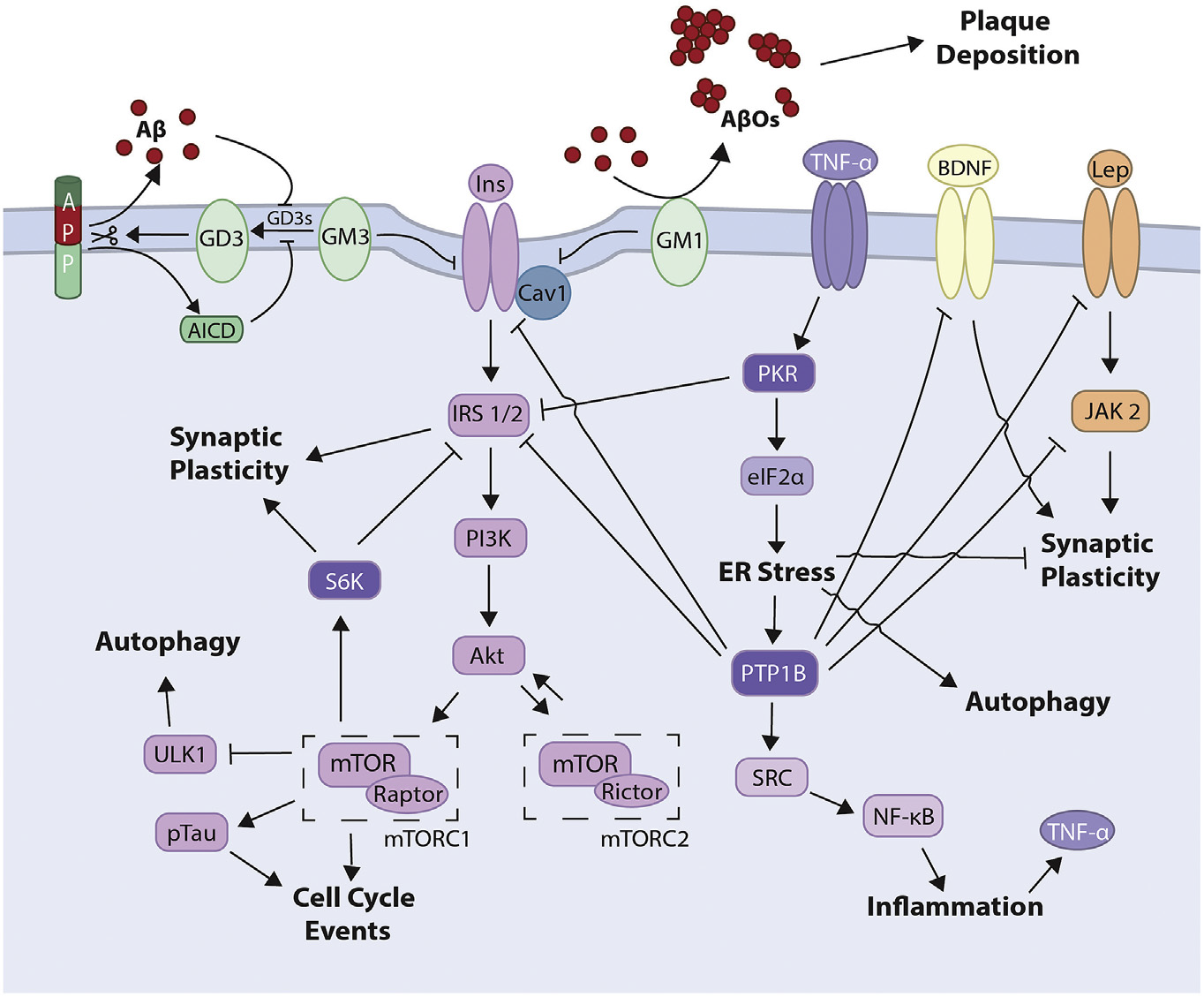
As is shown in this graphic from the journal article “Connecting Alzheimer’s disease to diabetes: Underlying mechanisms and potential therapeutic targets”, numerous pathways are involved in the connection from the insulin receptor onward. There are more obvious pathways: TNF-α is a major player in inflammation and well known to wreak havoc in disease states. Endoplasmic reticulum stress (ER stress) can result from a variety of conditions, whether it is unfolded proteins or stress in other organelles such as mitochondria. It also can severely limit a cell’s capability to function; in the case of Alzheimer’s disease, it significantly inhibits and limits pathways that typically expand synaptic plasticity, which is a process integral to learning and memory functions.
One particularly interesting area are the Aβ plaques that form on 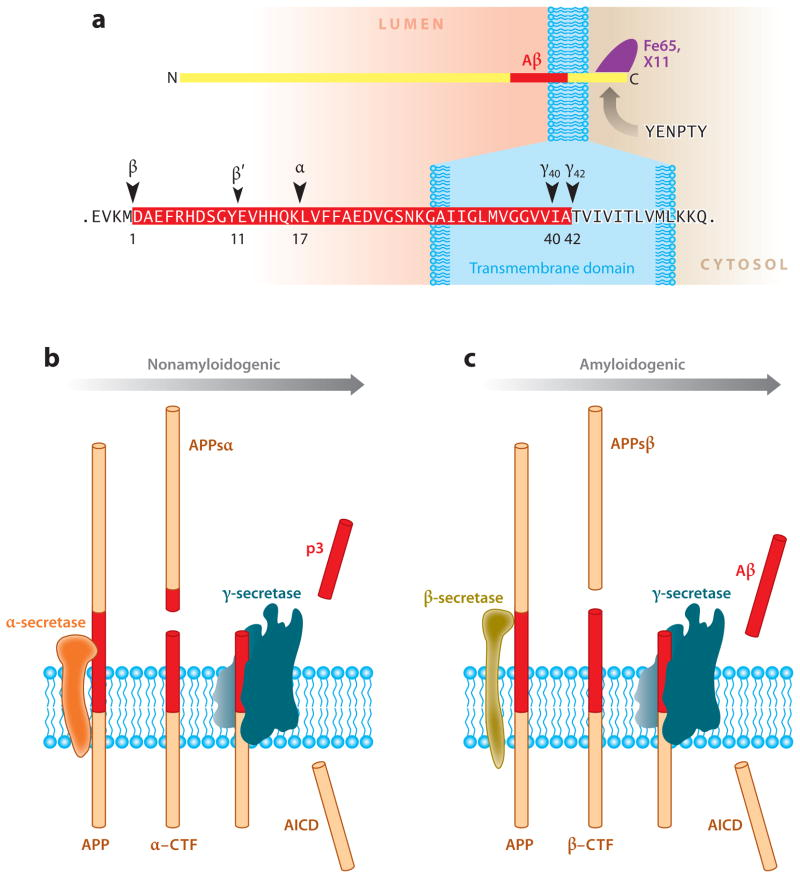 neurons. As the image to the right shows, the Amyloid precursor protein (APP) is a transmembrane protein in the brain that is a precursor to Aβs. Under certain conditions, APP is cleaved into p3. However, when another form of the secretase enzyme is used, the Aβs are formed. As these aggregate and continue to “clump” together, they form plaques on the neuron. That’s an interesting connection to Alzheimer’s disease, but how does this connect back to diabetes? Well, it turns out that the insulin degrading enzyme is involved in a complex that breaks down these Aβ plaques in the extracellular membrane. It is possible that in the drastically altered insulin functioning world of diabetes, these plaques are not being degraded efficiently or sufficiently.
neurons. As the image to the right shows, the Amyloid precursor protein (APP) is a transmembrane protein in the brain that is a precursor to Aβs. Under certain conditions, APP is cleaved into p3. However, when another form of the secretase enzyme is used, the Aβs are formed. As these aggregate and continue to “clump” together, they form plaques on the neuron. That’s an interesting connection to Alzheimer’s disease, but how does this connect back to diabetes? Well, it turns out that the insulin degrading enzyme is involved in a complex that breaks down these Aβ plaques in the extracellular membrane. It is possible that in the drastically altered insulin functioning world of diabetes, these plaques are not being degraded efficiently or sufficiently.
Why is this important?
As the video on Alzheimer’s disease suggested, understanding the science behind a disease on a molecular level is integral for developing effective treatments to target and potentially prevent said disease. Looking for connections among populations and searching for predispositions is an effective way to investigate potential pathways in common, giving both fields a greater understanding about the mechanisms of the disease and how that may connect to the body more globally. Especially with diabetes, it is essential to understand how it may lead to consequences later in life, with significant predisposition and risk for effects in the brain. Understanding these risks may help scientists and medical professionals give more sound advice to patients.
