Does your head hurt? Do you have a headache or sore neck? Are you sensitive to light and/or sound? These are just a few of the basic questions one gets asked while trying to make a diagnosis that lacks a more accurate way of assessment: a concussion. Otherwise known as a TBI (traumatic brain injury), it is something that most probably worry about getting after suffering a blow to the head or may be the reason altogether as to why parents steer their children towards a sport/activity with minimal contact. What exactly happens inside of the brain when it is suddenly thrown around, concussion or not? This will be explored below, as well as a term that may not regularly be incorporated with TBIs: myelin. Let’s keep reading!
A Journey Inside the Brain
Oh no! Your high school quarterback has just been diagnosed with a concussion from the football game last night. Thinking back to just seconds after he was hit  from behind, let’s examine what occurred microscopically inside of his brain as a result. The sudden movement inside his skull most likely started out with neurons becoming “leaky”, or more permeable for ions to flow in/out of the cell. For TBIs, there is an extreme influx of calcium and sodium ions with an efflux of potassium ions.
from behind, let’s examine what occurred microscopically inside of his brain as a result. The sudden movement inside his skull most likely started out with neurons becoming “leaky”, or more permeable for ions to flow in/out of the cell. For TBIs, there is an extreme influx of calcium and sodium ions with an efflux of potassium ions.
This sets off a series of reactions, starting with glutamate being released from these neurons and the cell uses up much of the ATP it has stored inside. This shortage results in the cell needing to generate more ATP to maintain other crucial reactions within the cell which creates a state known as hyperglycolysis. The lack of oxygen entering the 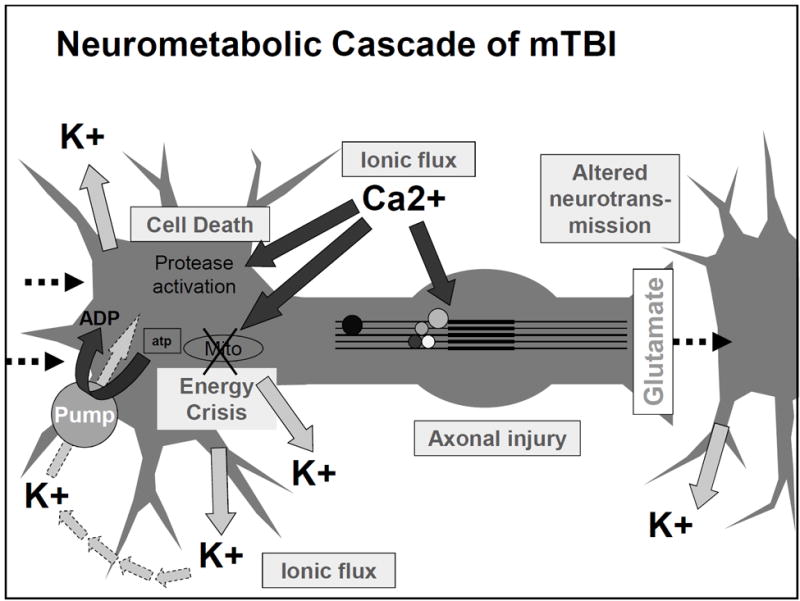 body compared to the amounts being consumed intracellularly results in an unfavorable side product being formed with ATP (lactate) and extra calcium getting stored in the mitochondria. Shrinking and running out of options, these cells quickly realize that they are now only doing more harm than benefit and decide to turn to apoptosis: programmed cell death.
body compared to the amounts being consumed intracellularly results in an unfavorable side product being formed with ATP (lactate) and extra calcium getting stored in the mitochondria. Shrinking and running out of options, these cells quickly realize that they are now only doing more harm than benefit and decide to turn to apoptosis: programmed cell death.
And to think- all of this is happening before he even stands back up from getting tackled.
Good Old Myelin
So now you probably are still curious about the cliffhanger I left you with from the beginning about this “myelin” stuff and how that plays a role in the brain and TBIs. Myelin is what wraps around the axons of neurons not only to help propagate action potentials, but also towards generating plasticity and cognitive abilities in the brain. Damage to these areas can result in a slower processing speed due to signal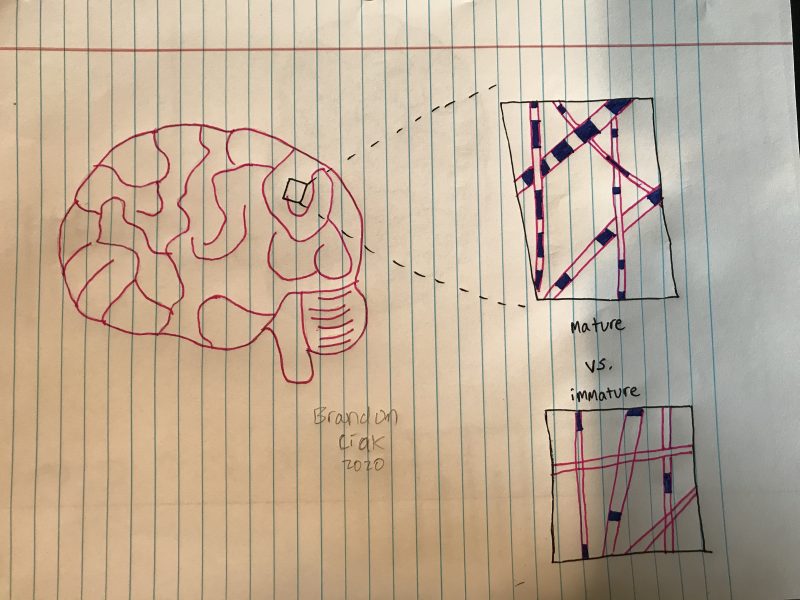 disruptions. Interestingly, humans are born with a pretty unmyelinated central nervous system, and so myelination is not something that is present until after our first couple years, which after still continues to contribute towards thickening the protective layers around individual axons in the ever-maturing brain. Different areas of the brain develop myelinated axons at different speeds, making it a very unfortunate scenario when an individual may develop a TBI in a place that is just underdeveloped compared to the rest.
disruptions. Interestingly, humans are born with a pretty unmyelinated central nervous system, and so myelination is not something that is present until after our first couple years, which after still continues to contribute towards thickening the protective layers around individual axons in the ever-maturing brain. Different areas of the brain develop myelinated axons at different speeds, making it a very unfortunate scenario when an individual may develop a TBI in a place that is just underdeveloped compared to the rest.
Takeaway message: Younger individuals have less myelination in their brain and a more flexible set of axons, but this results in a higher vulnerability for damage to occur, therefore this ultimately leads to cellular dysfunction and/or apoptosis.
Looking Ahead
Sadly, rest is the current go-to “antidote”, as there remains no over-the-counter medication that can be prescribed for individuals suffering from TBIs. Future advancements that are being developed with the growth of technology and science give optimism for things such as biomarkers to be not-so-much of a distant thought or conversation to be had.
Source of image: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4479139/