Is Metabolic Syndrome the same as Obesity?
Metabolic syndrome is defined as a cluster of conditions that occur together, increasing your risk of heart disease, stroke, and type 2 diabetes. Some of these conditions could include high blood pressure, high blood sugar, excess body fat, and abnormal triglyceride or cholesterol levels. All these conditions, together, lead to metabolic syndrome. But just because someone suffers from high blood pressure or abnormal cholesterol levels doesn’t mean they also have metabolic syndrome. However, any of these conditions increase a person’s risk of having metabolic syndrome.
So, obesity is considered a symptom of metabolic syndrome. They are not one in the same. And just because a person is obese, just like I mentioned above, doesn’t mean that they suffer from metabolic syndrome. Even vice versa, if a person is at a healthy weight, they may suffer from metabolic syndrome. This can be seen below, pictured in Figure 1.[1]

What’s the cause of these symptoms?
According to Alexander Jais and Jens C Bruning, “obesity has been known to induce a state of systemic low-grade inflammation that contributes to the development of numerous comorbidities.”[2] Not only can inflammation lead to many of these health-related issues, but it can also cause major changes in the brain, specifically in areas that keep homeostasis and systematic metabolism in check.
But what starts inflammation? A high fat diet leads to inflammation in the brain, as well as insulin and leptin resistance which will be discussed more later. A diet high in fat consists of pastries, biscuits, creams, cheese, cheese crackers, and many types of popcorn. Although eating these foods may be a contributing factor, it all depends on moderation.
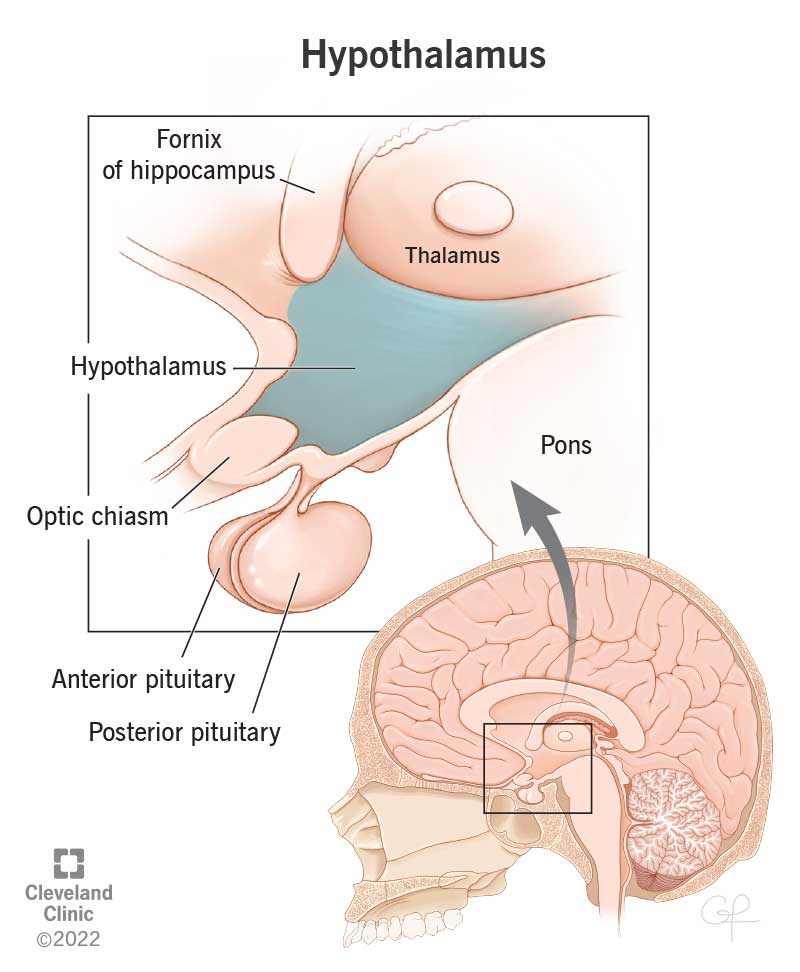
More specifically, hypothalamic inflammation is the main link to the development of metabolic syndrome. The hypothalamus is a structure that is located deep within the structure of the brain, it can be seen in Figure 2. The hypothalamus plays a major role in the body; it acts as the body’s “smart control coordinating center.”[3] The hypothalamus controls many neuroendocrine functions, or the relationship that occurs between the nervous system and endocrine system. These functions help to regulate energy homeostasis.
Insulin and Leptin
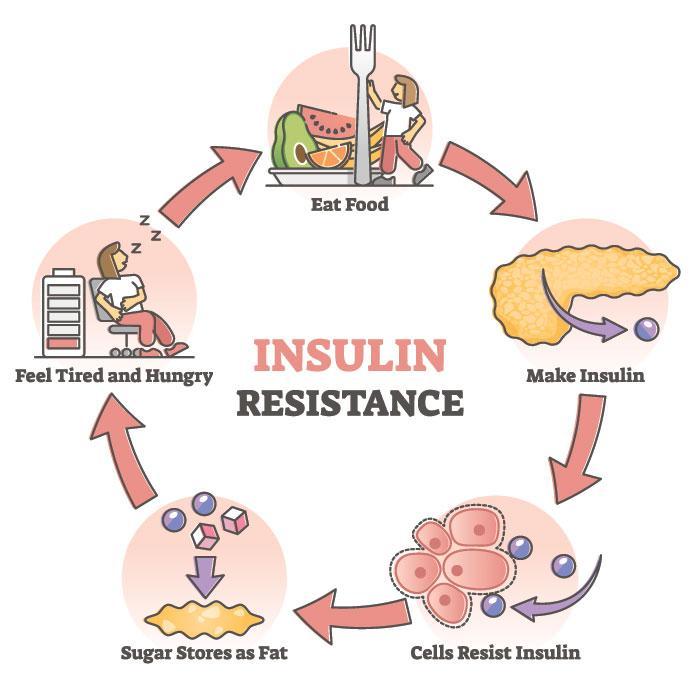
As previously mentioned, leptin and insulin levels are both affected by a high fat diet. Leptin is a hormone that helps to regulate energy levels by directing the central nervous system to adjust food intake accordingly. In other words, leptin tells the body when to stop eating and if leptin become dysregulated, a person may not know when to stop. The hormone insulin has a similar role. Insulin’s main role is to regulate the amount of sugar in the blood. When insulin is dysregulated, this most likely leads to high blood sugar which, as previously stated, leads to metabolic syndrome in many people. [4] [5]

Healthy lifestyle changes
- Choose heart healthy foods (fruits, vegetables, whole grains. Limit alcohol, sugars, and saturated fats)
- Exercise regularly
- Manage stress
- Don’t smoke
- Get enough sleep
- Medications for weight loss, cholesterol, blood sugar, blood pressure, etc. [6]
So, what?
Why should you care about any of this information? Well, in the United States alone, 1 in 3 adults suffer from metabolic syndrome. Although, most people don’t even know that they have this condition. So, it’s important to understand the risk factors and to take care of yourself. Statistically, you know someone with this disease. A person who leaves metabolic syndrome untreated will have a shorter lifespan than a person without the disease, the body must work much harder. Keep your body happy and healthy, it’ll love you for it. [7]

References
[2] Hypothalamic inflammation in obesity and metabolic disease
[4] Leptin and Leptin Resistance