 Artstract on DALL.E
Artstract on DALL.E
Metabolic syndrome, a cluster of conditions including obesity, high blood pressure, high blood sugar, and abnormal cholesterol levels, has been shown to have significant effects on the gut microbiome. Studies have found that individuals with metabolic syndrome have a less diverse microbiome, with decreased abundance of beneficial bacteria and increased abundance of harmful bacteria. These changes in the microbiome have been linked to increased inflammation, insulin resistance, and other aspects of metabolic syndrome. Additionally, some research suggests that alterations in the microbiome may contribute to the development of metabolic syndrome. Further studies are needed to fully elucidate the complex relationship between metabolic syndrome and the gut microbiome but targeting the microbiome may offer new avenues for treatment and prevention of metabolic syndrome [1].
Hypothalamic Microglia and Metabolic Syndrome
Hypothalamic microglia are a type of immune cell found in the hypothalamus region of the brain, which plays a crucial role in regulating metabolism and energy balance. In Metabolic syndrome, chronic low-grade inflammation can occur in the hypothalamus, leading to dysfunction of hypothalamic microglia, and subsequently, metabolic dysregulation. These activated microglia can release pro-inflammatory cytokines and reactive oxygen species, which impair the function of hypothalamic neurons and promote insulin resistance, obesity, and other components of Metabolic syndrome. Modulating the function of hypothalamic microglia could potentially be a therapeutic target for treating Metabolic syndrome and associated diseases [2].
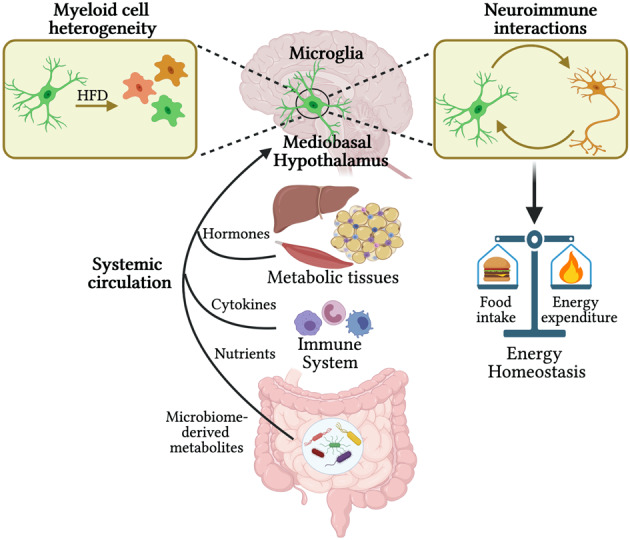
Figure 1. Factors impacting myeloid cells in the MBH to regulate hypothalamic control of energy homeostasis
Social and Environmental Factors
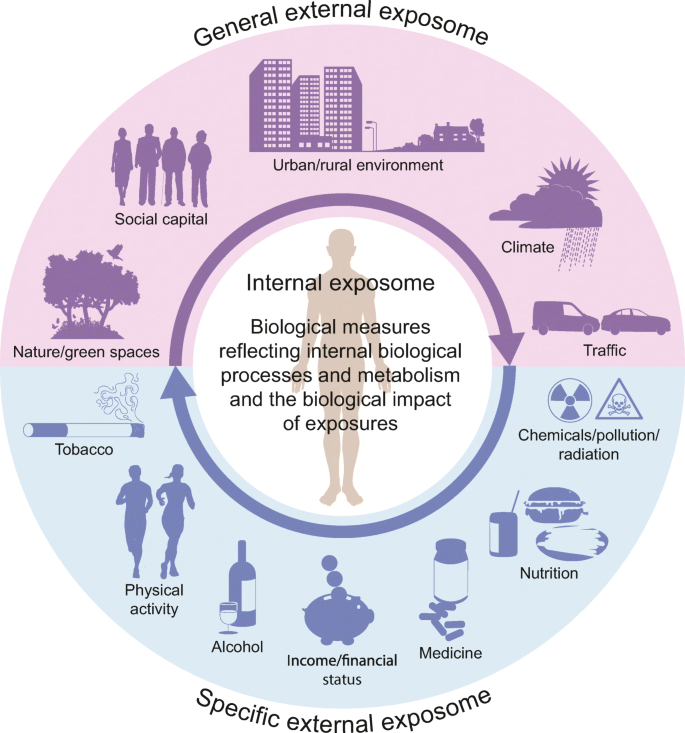
Metabolic syndrome is influenced by a variety of social and environmental factors. Lifestyle factors such as physical inactivity, unhealthy diet, and stress can contribute to the development of metabolic syndrome. In addition, social determinants of health such as low socioeconomic status and limited access to healthcare can also increase the risk of metabolic syndrome. Environmental factors such as pollution and exposure to endocrine-disrupting chemicals may also play a role in the development of metabolic syndrome. Addressing these social and environmental factors through public health policies, community-based interventions, and individual behavior change may help reduce the burden of metabolic syndrome and related health complications [3].
Vegetable oils, such as corn, soybean, and canola oil, have been linked to an increased risk of obesity. These oils are high in omega-6 fatty acids, which are pro-inflammatory and can promote insulin resistance, a key factor in the development of obesity and metabolic syndrome. Additionally, these oils are often used in processed and fried foods, which are high in calories and may contribute to overconsumption. Replacing these oils with healthier fats, such as olive oil or avocado oil, may have beneficial effects on weight and overall health. Reducing the intake of processed and fried foods, in general, can also promote a healthier diet and lower the risk of obesity.
Processed sugar is a major contributor to the obesity epidemic. Consuming large amounts of sugar, particularly in the form of sugary drinks and processed foods, can lead to weight gain and other health complications. Excess sugar intake can contribute to insulin resistance, a key factor in the development of obesity and metabolic syndrome. Sugar also lacks important nutrients and can displace more nutrient-dense foods in the diet, leading to overall poor dietary quality. Reducing the intake of processed sugar is an important step in preventing and managing obesity, and can have numerous other health benefits.
Figure 2. Social and Environmental Factors
Interventions
Lifestyle interventions such as diet modification, regular exercise, and weight loss are the first-line treatments for metabolic syndrome. Medications may also be used to control blood pressure, blood sugar, and cholesterol levels. In addition, some studies have shown that certain supplements and herbs, such as omega-3 fatty acids, probiotics, and green tea, may have potential benefits in managing metabolic syndrome. Bariatric surgery may also be considered in individuals with severe obesity and metabolic complications. Overall, the treatment of metabolic syndrome requires a multifaceted approach that addresses both lifestyle factors and medical management [5].
Resources
[1] Jais, A., & Brüning, J. C. (2017, January 3). Hypothalamic inflammation in obesity and metabolic disease. The Journal of Clinical Investigation. Retrieved May 1, 2023, from https://doi.org/10.1172/JCI88878
[2] Folick, A., Cheang, R. T., Valdearcos, M., & Koliwad, S. K. (2022, April). Metabolic factors in the regulation of hypothalamic innate immune responses in obesity. Experimental & molecular medicine. Retrieved May 1, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9076660/
[3] Ghosh, S., Dhar, S., Bhattacharjee, S., & Bhattacharjee, P. (2023, April 11). Contribution of environmental, genetic and epigenetic factors to obesity-related metabolic syndrome – the nucleus. SpringerLink. Retrieved May 1, 2023, from https://link.springer.com/article/10.1007/s13237-023-00420-y
[4] Beulens, J. W. J., Pinho, M. G. M., Abreu, T. C., den Braver, N. R., Lam, T. M., Huss, A., Vlaanderen, J., Sonnenschein, T., Siddiqui, N. Z., Yuan, Z., Kerckhoffs, J., Zhernakova, A., Brandao Gois, M. F., & Vermeulen, R. C. H. (2021, November 18). Environmental risk factors of type 2 diabetes-an exposome approach – diabetologia. SpringerLink. Retrieved May 1, 2023, from https://link.springer.com/article/10.1007/s00125-021-05618-w
[5] Saboya, P. P., Bodanese, L. C., Zimmermann, P. R., Gustavo, A. da S., Macagnan, F. E., Feoli, A. P., & Oliveira, M. da S. (2017, January). Lifestyle intervention on metabolic syndrome and its impact on quality of life: A randomized controlled trial. Arquivos brasileiros de cardiologia. Retrieved May 1, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5245849/