Obesity
Obesity is an extremely dangerous and costly condition affecting 41.9% of US adults and 19.7% of US children and adolescents. This is not just as issue in the US; obesity also affects 650 million adults worldwide [1]. These statistics are alarming, but even more concerning is the fact that these numbers are expected to increase significantly in the coming years. How is it possible that so many people are being affected by this condition? Aside from obvious genetic, epigenetic, and environmental influences, the key stimulus that kickstarts the metabolic changes associated with obesity is overnutrition which leads to altered chemical signaling within the body [2].
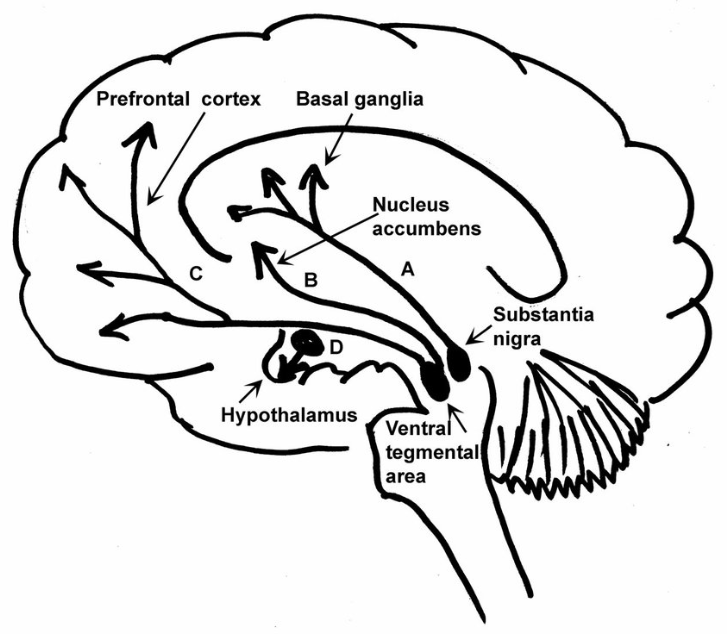
Food intake affects and is affected by two sets of neural pathways (Figure 1) within the melanocortin system of the hypothalamus. These two pathways lead to behavioral expressions of energy expenditure and caloric intake with the goal of maintaining nutritional homeostasis. The agouti-related peptide (AGRP) pathway is orexigenic, meaning it induces feeding, and it works antagonistically to the anorexigenic proopiomelanocortin (POMC) pathway which restricts feeding behaviors. Insulin and leptin are hormones that are released following food intake to inhibit AgRP neurons and activate POMC neurons. This sends neural signals to decrease food intake while increasing energy expenditure to limit overnutrition. When insulin and leptin are no longer present in the receptors, feeding behavior will be triggered and energy expenditure should decrease. [2].

Signaling Dysruption
Insulin and leptin signaling dysregulation are one of the first changes that occur in the development of metabolic syndrome and obesity. Just three days of feeding on a high fat diet can significantly reduce hypothalamic insulin sensitivity. This occurs when the insulin receptors are receiving too much input. When there are too many signaling molecules trying to bind to receptors, the receptors become desensitized to the constant stimulation of insulin. When insulin sensitivity is reduced, anorexigenic signals are not able to be properly sent to the brainstem (Figure 1). This not only induces more feeding behavior leading to body weight gain, but also leads to a state of hyperinsulinemia which produces other negative effects [2,3].
High fat diets also affect other signaling pathways in the hypothalamus. Proinflammatory gene expression in the hypothalamus occurs via the IKK complex and NF-kB activation. High fat diets also can impair insulin action by phosphorylating and inhibiting the insulin receptor substrate proteins at serine 307. This is another mechanism that promotes activation of the AgRP neurons (Figure 1) which induces over-eating behaviors [2].
The Cycle
Although there are many different mechanistic explanations for the changes we see in hypothalamic signaling, they all come from the same stimulus and produce similar behavioral and physiological responses. High fat diets are the impetus for each of these metabolic alterations, and each of these alterations produce negative effects of insulin/leptin resistance, increased food consumptions, inflammation, and eventual weight gain. When a high fat diet is consumed regularly, both the acute and long-term effects perpetuate the same behaviors – over fueling and under activity.
The inflammation associated with obesity specifically affects the brain structures involved in reward and feeding behaviors. Because of this, the reward pathways in the brain seek out more highly-palatable high fat foods, further perpetuating this cycle. Inflammation also affects peripheral tissues and organs within the body leading to negative effects in other body systems.
Conclusion
Through all of the signaling, chemical, metabolic, and behavioral changes that occur with obesity, the most important thing to understand is that they are all connected. Once the cycle of obesity is initiated, it continues to perpetuate itself through all of the mechanisms discussed above. This process is usually initiated by dietary choices and often is not stopped unless deliberate action is taken. The first step in ending the cycle of obesity is bringing awareness to the problem and educating about how and why this is occurring.
References: