Schizophrenia is a complicated brain health condition that affects millions of people worldwide. But even though we know a lot about it, we still don’t fully understand what causes it. That being said, recent research has zeroed in on the Wnt signaling pathway and its connection to Glycogen Synthase Kinase 3 (GSK3) as key players in brain development and schizophrenia. Understanding how these pathways work doesn’t just help us understand the science behind schizophrenia, it also opens doors for new treatment options.
The Role of Wnt in Building a Healthy Brain
The Wnt signaling pathway is kind of like a traffic control system for brain development. It helps guide important processes like cell differentiation, neuron formation, and survival. There are two main branches:
-
The canonical pathway, which controls gene expression through β-catenin.
-
The non-canonical pathways, which regulate things like cell movement and calcium signaling.
Normally, when Wnt isn’t around, GSK3β tags β-catenin for destruction before it can activate any genes. But when Wnt binds to its receptors (Frizzled and LRP5/6), β-catenin is protected from being broken down. This allows it to reach the nucleus, where it turns on genes crucial for brain function.

Figure 1. This shows the wnt signaling pathway, specifically the canonical signalng where Wnt binds Frizzled (FZ) and LRP5/6, activating Disheveled (DVL) and inhibiting β-catenin degradation. Stabilized β-catenin enters the nucleus, activating gene expression.
How the Environment Affects Wnt and Schizophrenia
It’s not just genetics that shape brain health. Environmental factors can mess with Wnt signaling too, especially before birth. Things like prenatal infections, malnutrition, and toxin exposure can alter Wnt-related gene expression, which can rewire the brain in ways that increase schizophrenia risk.
For example, if a pregnant person gets an infection, their immune response can disrupt Wnt/GSK3 signaling in the developing brain, leading to changes similar to what we see in schizophrenia patients[1]. And it’s not just infections—pollutants like heavy metals and endocrine disruptors have been found to impact the epigenetic regulation of Wnt genes, which could contribute to the disorder later in life[2].
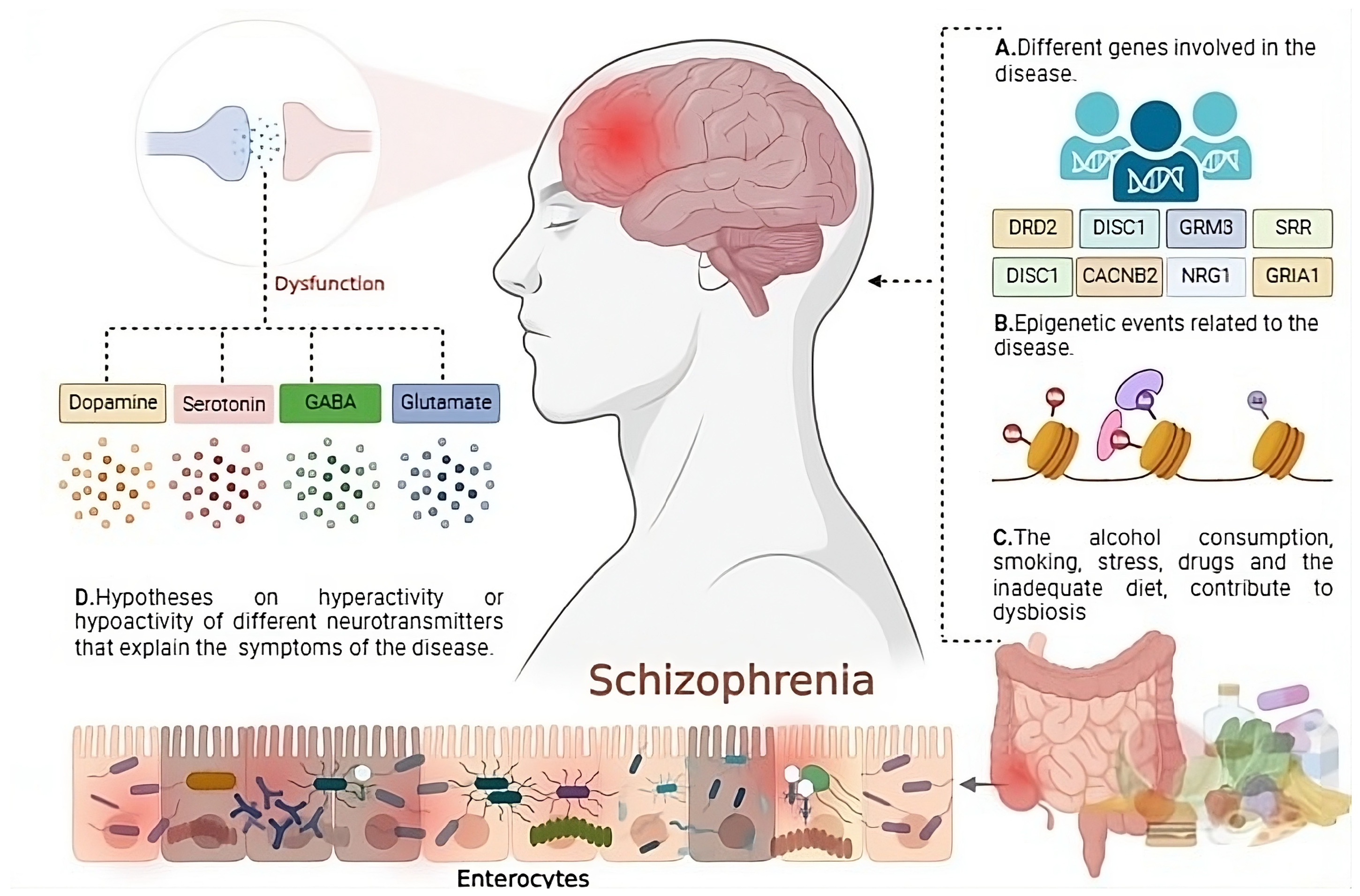
Figure. 2. this demostrates how schizophrenia arises from genetic factors (e.g., DRD2, DISC1, GRM3), epigenetic modifications, and environmental influences (e.g., stress, diet, substance use) affecting the gut, immune, and brain systems. Dysregulation of dopamine, serotonin, GABA, and glutamate contributes to symptoms.
Can We Lower the Risk of Schizophrenia?
While genetics play a role, research shows that lifestyle and environmental choices might help lower the risk. Some key strategies include:
-
Prenatal Care: Getting proper medical care during pregnancy, including vaccines and good nutrition, may help protect fetal brain development.
-
Reducing Toxin Exposure: Avoiding harmful chemicals like lead and pesticides could help keep Wnt signaling on track.
-
Dietary Support: Nutrients like omega-3s, folate, and vitamin D have been linked to healthy Wnt activity and brain growth[3].
-
Early Intervention: Spotting early signs of schizophrenia risk could lead to targeted treatments, like cognitive training or medications that support Wnt signaling[4].

Artstract created by S. Mohamed
Schizophrenia is still full of unknowns, but the more we learn about the Wnt and GSK3 pathways, the closer we get to better treatments and even prevention strategies. Understanding brain health on a molecular level is the first step toward changing the way we see and treat mental illness.
Footnotes
[1] Singh KK. An emerging role for Wnt and GSK3 signaling pathways in schizophrenia. Clin Genet. 2013; 83(6): 511-517.
[2] De Ferrari GV, Moon RT. The ups and downs of Wnt signaling in prevalent neurological disorders. Oncogene. 2006; 25(57): 7545–7553.
[3] Chenn A, Walsh CA. Regulation of cerebral cortical size by control of cell cycle exit in neural precursors. Science. 2002; 297(5580): 365–369.
[4] Gould TD, Einat H. β-catenin overexpression in the mouse brain phenocopies lithium-sensitive behaviors. Neuropsychopharmacology. 2007; 32(10): 2173–2183.