
Artstract created S. Mohamed
Addiction is not a choice. It’s a complex brain disease. And for millions of people struggling with psychostimulant use—cocaine, meth, nicotine, and amphetamines—it can feel like there’s no way out. While we know these drugs hijack the brain’s reward system, we’re still uncovering how they reshape it at the molecular level. Until now, there hasn’t been a strong therapeutic target to reverse these brain changes and truly help people recover. But new research offers a powerful insight: a group of brain receptors called metabotropic glutamate receptors (mGluRs) might be the key to healing the brain after drug abuse.
Therefore, understanding how these receptors work could change the way we treat—and talk about—addiction. Let’s unpack how psychostimulants mess with our brain chemistry and why that makes addiction less of a choice and more of a brain health issue.
The Reward Circuit and Dopamine: Why Drugs Feel Good
Dopamine is the brain’s “feel-good” chemical. It spikes when you experience something pleasurable like eating chocolate, getting a compliment, scrolling TikTok at 1 a.m. It also spikes when someone uses a drug. And that’s where the problem starts.
Dopamine plays a huge role in the brain’s reward system, which includes areas like the ventral tegmental area (VTA), nucleus accumbens (NAc), and prefrontal cortex (PFC). When dopamine floods this system, the brain takes note: “This felt good. Let’s do it again.” Over time, your brain builds tolerance, needing more and more of the drug just to feel normal.
But there’s another layer: the brain learns to expect dopamine in certain contexts maybe it’s a particular room, a group of friends, or even a certain time of day. These environmental triggers can increase tolerance or make someone more likely to relapse. And when the drug is taken outside of that context, the body isn’t ready leading to accidental overdose[2].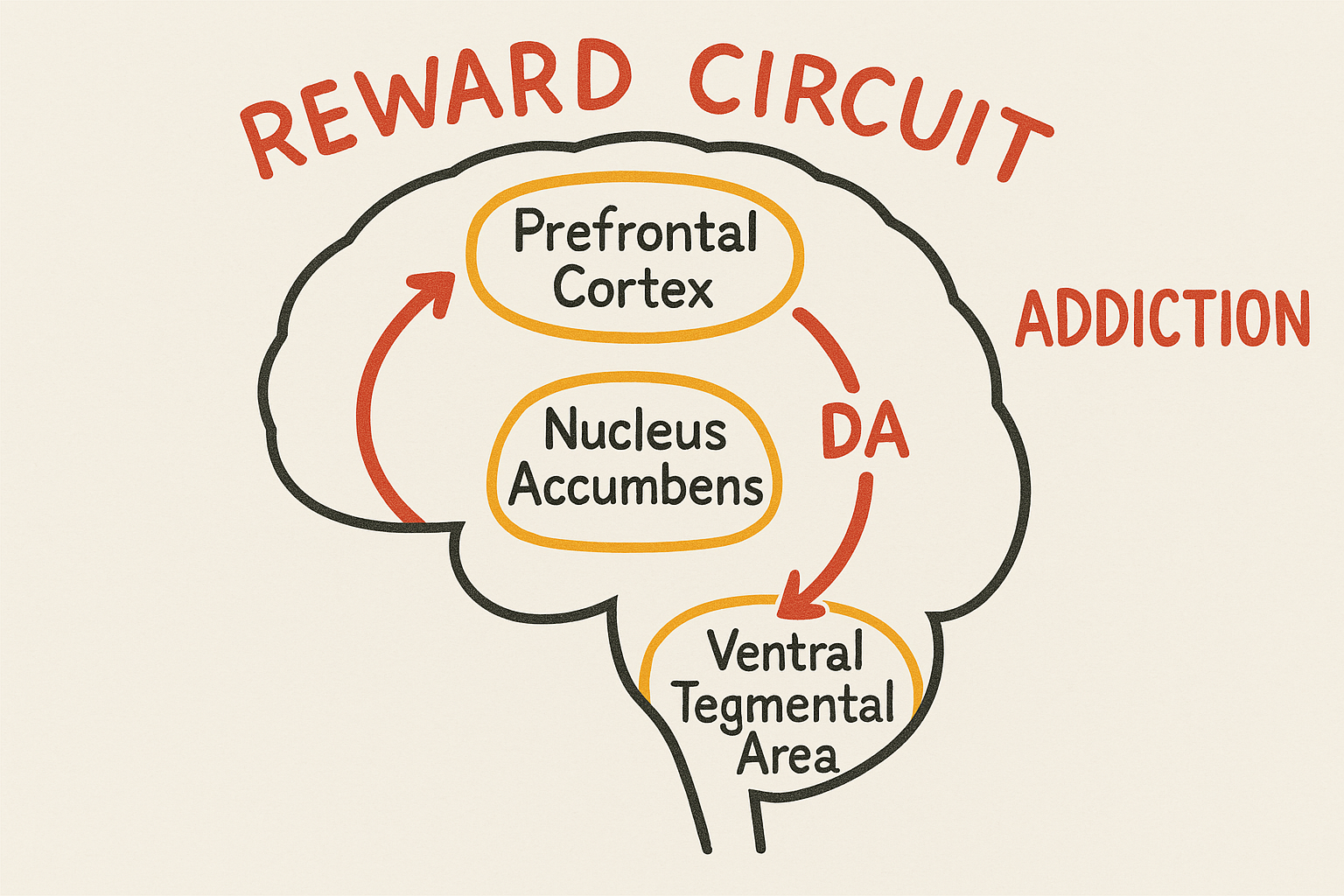
Figure[1]. This figure illustrates the brain’s reward circuit connecting the prefrontal cortex, nucleus accumbens, and ventral tegmental area via dopamine signaling and how its dysregulation contributes to addiction.
Glutamate: Reinforcing the Habit
While dopamine makes drugs feel good, glutamate helps the brain remember how good it felt.
Glutamate is the brain’s main excitatory neurotransmitter. It’s essential for learning, memory, and synaptic plasticity a fancy term for how the brain strengthens or weakens connections between neurons. Drugs like cocaine, nicotine, and amphetamine increase glutamate levels and hijack these learning processes.
They do this by activating metabotropic glutamate receptors (mGluRs)—especially Group I receptors like mGluR1 and mGluR5. These receptors become overexpressed or relocated to different parts of neurons. For example, mGluR5 increases in the prefrontal cortex, while mGluR1 spreads into extrasynaptic sites, both changes linked to long-term neuroplasticity in addiction[1].
The result? The brain gets really good at learning how to crave drugs and not so great at resisting them.

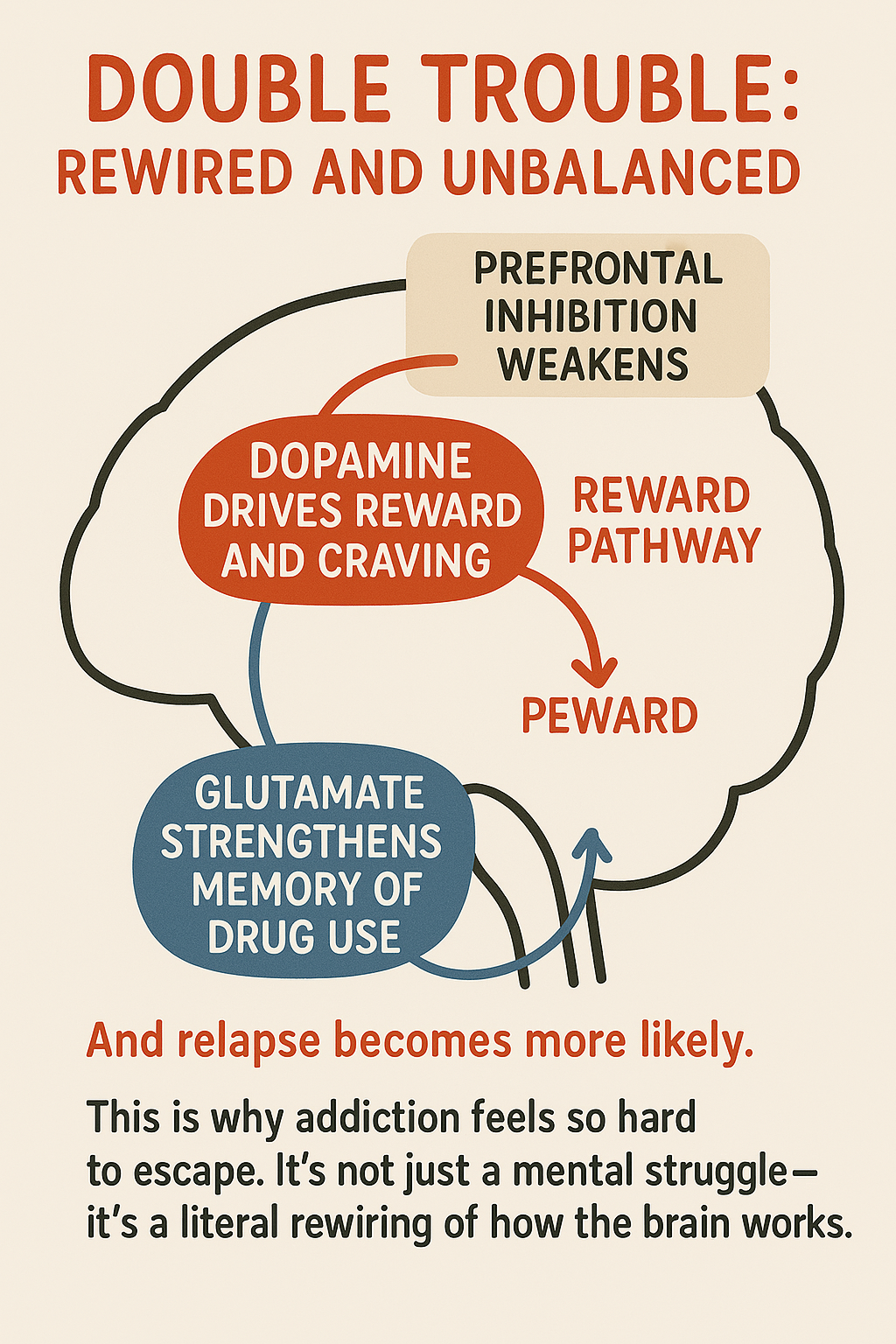
Figure [2]. Brain regions and synaptic pathways involved in addiction, showing how Group I, II, and III mGluRs differentially modulate glutamatergic and dopaminergic signaling.
Double Trouble: Rewired and Unbalanced
Normally, your prefrontal cortex helps with decision-making and impulse control. But repeated drug use weakens this system. The brain keeps getting messages like this drug is great from the reward pathway, while the logical part of your brain can’t shut it down.
So… Can the Brain Ever Go Back?
The scary thing about addiction is how good the brain becomes at remembering drugs. But the hopeful part? The brain is also capable of change. Researchers have found that those same metabotropic glutamate receptors (mGluRs) that help reinforce drug memories might also hold the key to reversing them. By targeting these receptors, it may be possible to rebalance the brain’s glutamate system, reduce cravings, and actually “unlearn” the cycle of addiction.
Here’s what’s exciting:
-
Blocking mGluR5 reduces drug-seeking and relapse in animal studies.
-
Activating mGluR2/3 helps calm excessive glutamate and lowers craving.
-
These strategies work across multiple substances like cocaine, meth, nicotine, and more.
And most importantly, these treatments don’t just patch over symptoms. They work at the cellular level, where addiction takes root. They aim to restore balance in how the brain learns, remembers, and responds to reward.
Addiction Is Brain Health
So yeah, drug use and addiction is scary. It rewires how the brain is rewarded, how the brain learns, and how much impulse control a person has. But the biggest takeaway here is that addiction is not just bad choices—it’s bad brain chemistry.
Understanding the science helps us reframe the narrative. Addiction isn’t a personality flaw. It’s a brain disorder that deserves real treatment and real compassion. The more we know about glutamate, dopamine, and mGluRs, the closer we get to treating addiction like the health condition it truly is.
References:
- Mozafari, R., et al. (2023). A review on the role of metabotropic glutamate receptors in neuroplasticity following psychostimulant use disorder. Progress in Neuropsychopharmacology & Biological Psychiatry.
- Siegel, S. (2001). Drug tolerance, cue exposure, and overdose. Addiction Research & Theory, 9(5), 411-419.
- Kalivas, P. W., & Volkow, N. D. (2005). The neural basis of addiction: A pathology of motivation and choice. Am J Psychiatry, 162(8), 1403-1413.