Where are my keys?
“Oh no, I misplaced my keys yet AGAIN this week. My memory must be going. But wait. Does this mean..Could I possibly have..It couldn’t be..Alzheimer’s Disease?” Alzheimer’s disease (AD) is the sixth leading cause of death in the United States with an alarming and increasing mortality rate. With the vast number of improvements in healthcare within the past decade, mortality rates of various leading causes of death in the United States, including heart disease, various cancers, and diabetes have decreased; but the mortality rate of AD continues to climb due to the lack of a cure and effective medication to prolong the lives and cognitive functioning of AD victims. Many people today are haunted by the questions “Am I at risk for developing AD?” and “Why is this disease so fatal and difficult to cure?”
Celebrating another year of life and an increased risk for AD
AD is often attributed to genetic factors when genetically inherited forms of AD are actually extremely rare. Scientists have realized that the true cause of AD is still unknown today. There are many factors that play into AD development, including diet, exercise, diabetes, cardiovascular disease, and other environmental and genetic factors. But recently, aging has been highlighted as the major risk factor in the development of AD. But why?
It is due to abnormal control of a specific pathway in the brain called the P13-K/Akt signaling pathway. This pathway is associated with cell growth, proliferation, and consequently healthy aging and longevity when its activity is carefully regulated. Lack of normal control of this pathway is also involved in many other major diseases, including cancer, type 2 diabetes mellitus, heart disease, and neurodegeneration. So, what is going wrong in this pathway to cause AD and its characteristic symptoms of cognitive decline and memory loss?

Figure 1. The interconnectedness of genetic and environmental factors that play into cognitive decline present in AD.
Leaving the light on in the AD Brain
The P13-K/Akt signaling pathway is carefully regulated in a healthy brain, meaning that it is turned on and off in response to various molecular signals or processes to promote healthy cell proliferation, growth, and functioning. This can be compared to turning on and off the lights in the living room of a home. In order to conserve energy and money (via the payment of a monthly electric bill), many people will turn the living room lights on when they are in the room and will turn the lights off when they are no longer in that room. The P13-K/Akt pathway is overactive in the AD brain and it is not being shut off; this is similar to leaving the lights on in the living room, even when no one is in the room.
The P13-K/Akt pathway is initially activated by insulin. When insulin binds to and activates its receptor in the membrane of a cell, it leads to a phosphorylation cascade within the cell, or the activation of a number of enzymes in a specific order via the addition of phosphates onto those enzymes. The activation of the insulin receptor eventually leads to the activation of P13-K and ultimately the activation of Akt. The activation of Akt leads to a variety of molecular processes. When activated, Akt acts as both an activator and deactivator of a variety of enzymes. The actions of Akt consequently result in a lack of anti-stress response (which is needed for our body and brain to respond to stress in a healthy way) and prevention of its own (Akt) inactivation. Both of these results contribute to the lack of regulation of the P13-K/Akt pathway seen in AD brain. When this P13-K/Akt pathway is overactivated, it ultimately leads to insulin resistance, similar to that seen in type 2 diabetes mellitus due to unhealthy diet habits. When this pathway is constantly ON (which is not normal in a healthy brain), the body attempts to compensate for this over-activation by reducing the number of insulin receptors in the membrane of cells. With less receptors to respond to insulin, there is less activation of the pathway. However, this often leads to complete insulin resistance in the brain, which is fatal due to the high energy needs of brain cells.
 Figure 2. Depiction of unhealthy eating habits leading to insulin resistance and the formation of Alzheimer’s disease.
Figure 2. Depiction of unhealthy eating habits leading to insulin resistance and the formation of Alzheimer’s disease.
P13-K/Akt overactivation also leads to the hyperphosphorylation (too much phosphorylation) of a protein called tau in the brain. These phosphorylated tau proteins end up aggregating within brain cells and start to stick to each other, creating what is known as neurofibrillary tangles (NFTs). NFTs are characteristic of AD brain and they inhibit the functionality of neurons and neuronal communication within the brain. The presence of high numbers of phosphorylated tau proteins within brain cells also mediates the formation of extracellular amyloid-beta plaques, which is also characteristic of AD brain. These amyloid-beta plaques accumulate outside of the cell and bind to the insulin receptors of the P13-K/Akt pathway that are in the membrane of brain cells and activate the pathway (positive feedback). The impairment of neuronal communication and transmission of signals in the brain leads to memory impairment and cognitive decline, both of which are symptoms of AD.
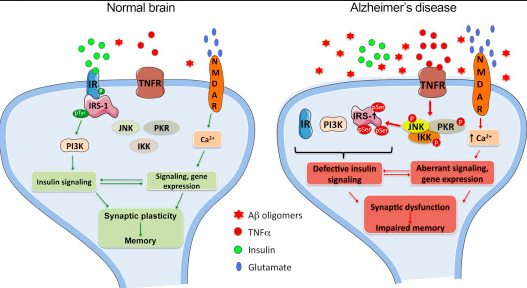
Figure 3. Comparison of a healthy, regulated P13-K/Akt pathway and a nonfunctional, non-regulated P13-K/Akt pathway seen in AD.
Healthy Body, Healthy Brain: The future of AD
AD is a major topic of current research and scientists are consistently learning more about the AD brain in order to develop a better understanding of the physiological processes occurring that lead to AD development in the brain. AD is a particularly difficult disease to study due to the complexities of studying a live human brain. Although there are current medications used to slow the progression of AD symptoms, such as memory loss and cognitive decline, there is still no proven prevention or cure. The only scientifically supported prevention for AD today is exercise and healthy eating. So maybe all of these new fitness programs aren’t so bad after all? Healthy body, healthy brain, who could complain? With the advancement of healthcare and scientific research, we hope to continue to develop a better understanding of the pathophysiology of AD that will aid in the creation of future AD preventions and cures. Although there is always hope in the future, there is no solid promise today.
If you would like to learn more information about the neurophysiological development of Alzheimer’s disease with aging, please visit:
http://www.sciencedirect.com/science/article/pii/S053155651300065X?via%3Dihub
Featured Image from:
http://www.pureherbalayurved.com.au/alzheimer-disease-ayurvedic-treatment-melbourne.htm
Images from:
http://www.biochemsoctrans.org/content/33/5/1041
http://www.sciencedirect.com/science/article/pii/S155252601302918X
