Obesity is sometimes viewed as a lack of discipline. The obvious fix is start eating healthier and work out a few times a week. Although eating right and exercising are very important, obesity is more than just a weight problem.
There are neurological components to this disease that is plaguing the United States. One component of this very complex illness is the dysregulations of signals being sent in one’s brain.
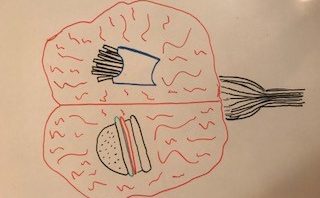
In the hypothalamus and brain stem, there are specialized neurons called proopiomelanocortin neurons or POMC neurons for short. These neurons are vital players in the story of food control. POMC neurons send projections throughout the brain that let you know you’re full and should stop eating. The POMC works in tandem with a peptide called the agouti-related peptide (AgRP). This peptide is responsible for the signal to eat.
One regulator of POMC is a hormone called leptin. Leptin flows through the blood and when it reaches the brain it binds to the POMC neurons, therefore sending a signal to stop eating. When this process is interrupted in rats, obesity is seen as a result. Other mutations to POMC can lead to adrenal failure, along with early on-set obesity. Therefore, it is evident that this process is vital for maintaining a healthy weight.
This result of over-eating can further damage the body by leading to insulin-resistance. When over nutrition occurs, it can lead to ER stress which activates a pathway called the JNK pathway. This pathway is an inflammatory pathway which ultimately ends in inhibiting the insulin receptor substrates. This inhibition therefore leads to insulin resistance as the insulin signal will no longer be able to be passed on down it’s cascade of signals.
Obesity is large problem in our country. This problem comes with a stigma that those individuals who are obese are weak and have control problems. However, when further examining the components of this disease there are many neurological components. It is an imbalance of chemicals and other peptides. Therefore, I believe that with more research obesity will shift to being seen as a brain disease as well, hopefully improving the treatment and reducing the incidence.
For more reading on obesity and the brain, please check out:
http://www.cell.com/trends/endocrinology-metabolism/fulltext/S1043-2760(12)00204-4
Obesity – More Than Self-Control?