Coming out of high school we all know how tough it is to decide what you want to do with your life or where you want to go. Being from Mesa, Arizona I only knew one thing…I wanted to leave there and see another part of the country. I visited schools in Iowa, Colorado, and in Minnesota and after 10 plus visits I finally settled at Concordia. I mean after all I was kind of a legacy at this school. My aunt is in the athletic hall of fame for winning a national championship here and my great grandfather is former Concordia College president Joseph Knutson (his statue is in the Knutson Campus Center). The decision was one of the best I have made in my life.

The first reason it was the best choice is that I got to continue to play the sport I love, but being able to put education first was key. I played golf at this college for four years, amassing 23 top-25s and finishing 3rd all-time in career scoring average. Most importantly though I was privileged enough to become captain the past two years and to be able to show the other men how to make the right choices. This allowed me to make an imprint on my fellow teammates and shape how they think about the world. It is important to stress the ability to instill a hard work ethic, the same work ethic that I learned in Chemistry 127-128 in my freshman year. Golf provided me an outlet and allowed me to grow as a man and a kid trying to become a responsibly engaged in the world.

The education at Concordia is grueling and the teachers are not shy about pushing you to exceed your expectations. They push you to set higher goals and expand your horizons. Dr. Mach of my Neurochemistry class has done this just as much as anyone. In her class we looked at 9 neurodegenerative diseases the plague the world at this time and each week I found myself becoming more engaged in the material and thirsting for more knowledge on the topics. In life, there is no easy road and I am constantly going to keep driving forward and the thirst for knowledge that Concordia has instilled in me will make that happen.
The well-rounded curriculum at Concordia College has allowed me to be a science major but also take classes in global studies, English, and humanities while also focusing on my major. This allows me to make connections between fields of study that I would not have had the ability to do at a large university. It has become easier for me to see problems from many different angles and has allowed me to see the world from a new lens. All this allows me to become a more responsible citizen in a global community.

Finally, we get to my capstone experience, the peak of the mountain, the cherry on top of the sundae. Taking Neurochemistry for any science major is a must. The ability to have a free flowing classroom where we all participate and are not lectured at for an hour provides an experience where we all learn together. We research was interests us and are not confined to a bubble of material that the professor assigns. Dr. Mach gave all of us the freedom to follow our passion and this was especially exemplified in the blog posts and the community action project. The blog posts only requirement was that they had to focus on the week’s topic and provide some science. This allowed me to write a biography one week and provide research another. These gave me the chance to provide my own learning into the topic.

The community action project was another highlight of my undergraduate education. Logan, Hannah, and I decided to focus on ALS a debilitating neuro disease that has no cure and is a death sentence. Based on Dr. Mach’s instructions whatever we did just had to be focused on ALS and this gave us the freedom to act as ambassadors to the ALS association and try and promote the ALS walk in Fargo, ND on Saturday August 19 at 10:00am. We contacted radio station executives in an effort to get air time to discuss the walk and are still in negotiations, but this experience allowed us to leave the bubble on campus and promote change on a larger scale. To experience the real world and try to make a difference. Hopefully we are successful in the end.

My time at Concordia has come and gone and I am thankful for the opportunity to attend a college that allowed me to grow as a man. A place where the professors push you to excellence, but at the same time provide you with the support needed. A place where I was able to follow my passion of playing golf and also provide me with a rigorous education. However, now it is time to enter the real world and I know wherever I go, Concordia has provided me with a launch pad into the future.

Am I Smarter for Going to a Fancy Pants School, or Did I Blow a Bunch of Money for Nothing?
Waiting till the last moment to reflect on my college education, in true Gus McCarthy fashion, I think my time spent at Concordia was worth the extra buck.
I’ve been asked to reflect on the mission of Concordia College by highlighting my experience with the five goals.
- Instill a love for learning
- Develop foundational skills and transferable intellectual capacities
- Develop an understanding of disciplinary, interdisciplinary, and intercultural perspectives and their connections
- Cultivate an ethical, physical, cultural, and spiritual self understanding
- Encourage responsible participation in the world
 The guy on the left here isn’t the dumbest person in the bunch, but he also has the worst study skills imaginable. He can understand subject matter, but transferring it is impossible, and he has no idea who he is.
The guy on the left here isn’t the dumbest person in the bunch, but he also has the worst study skills imaginable. He can understand subject matter, but transferring it is impossible, and he has no idea who he is.I didn’t have many life experiences prior to Concordia. I had invested heavily in my sports career, and I got good but not great grades. Everything ended up changing when I got to Concordia.
Autism Spectrum Disorder: It’s Zinc! No Wait, It’s Antibiotics! No, It’s….

Autism Spectrum Disorder, or as I will be using very frequently, ASD, is a very hot topic disorder these days because no two people are affected the same way. From this, we are blessed with the difficult task of trying to explain their symptoms, treat them, and help them assimilate into society as the rest of us all try to do. So how exactly is this possible? Fantastic question, I’m glad you asked because I have a slight understanding of how ASD works.

From working together to come up with an idea in class, we arrived upon an agreement that Zinc deficiencies play a significant role in development in utero (Shocking… I know…) We found that zinc is a cofactor in protein synthesis, cell division, and immunity for both mother and baby. I would go out on a limb and say that it is a big shock that we all aren’t slightly on the autism spectrum because it just does not seem like proper levels are stressed to pregnant mothers. After reading the labels on several assorted brands of prenatal vitamins, I was presently surprised to find that an acceptable amount of zinc is included in these supplements. Unfortunately, not all mothers are planning on having a child, so I can go to imagine that many future mothers are not properly preparing their bodies for a little bundle of joy.

The next hot topic issue we found was the treatment of mothers for infections during pregnancy and how it is such a double edge sword. On one hand, it is ridiculous to leave any infection untreated (if out of control) but at the same time, antibiotics are not necessarily the healthiest item to be passed along to a fetus. It has been found that children whose mothers were treated with antibiotics during pregnancy were more likely to develop symptoms resembling ASD. This connection was discovered through many of these children having a gut microbiome dysbiosis. Although it is a long shot to draw a strong correlation between the two, one should take these facts as a warning story before jumping to antibiotic use if it isn’t necessary.
*Insert Clever Title Regarding Parkinson’s Disease*

Parkinson’s disease is an interesting disorder that has many factors that contribute to its complexity. As most of us know, Parkinson’s is a well-publicized disease as there have been a few famous people that have brought a great deal of attention to raise awareness and funding to research it. Michael J. Fox has been a headliner in the battle to find a cure for Parkinson’s because he was diagnosed with it at such a young age. To his advantage, he has the ability to use his acting background to bring attention to the dire need of further research for this condition because there is not a cure.

One of the aspects of Parkinson’s that makes it so complex is the pathway in which it plays inhibits. The pathway that is affected is the motor movement pathway. This entire route of signaling involves several areas of the brain in which there is planning of the movement in the prefrontal cortex, the information from the prefrontal cortex is then used to activate the basal ganglia which is an enormous player in this pathway because it requires a great deal of dopamine to activate the next steps in the pathway. Much research supports the basal ganglia as being the problem location of the brain that has Parkinson’s because the neuronal cells require a great deal of dopamine to continue the signaling of the pathway. This essentially highlights one of the overarching issues of Parkinson’s disease because the main problem within the signaling cascade between neurons arises from an overall lack of Dopamine to use to excite the next cells down the line.

From the disorder of the motor controlling pathway, the common symptoms found can either be resting tremors of outer limbs to begin. Many patients come with a common symptom of a pill rolling tremor that looks exactly as it sounds. To give an example, think of when you were young and had to take a pill that looked way too big. So, what did you do? Most of us would imagine rolling it around between our thumb and index finger. This exact action is what a Parkinson’s patient would likely present with either in early or late stages of the disorder. Additionally, it is important to recognize that Parkinson’s is a developing disorder that begins in the external parts of our bodies as it may begin in our feet as well as our hands and slowly work its way around in the body. Also, coming from Parkinson’s as a symptom that contrasts the resting tremors is the inability to generate movements in various limbs. Another example that can be commonly seen with the failure to generate movement can be found with these patients being unable to make the first movements when it comes to walking. This too arises from the disorder of the motor movement generating area of our brains and it results from the motor cortex being unable to be stimulated.

Brains Are Cool. Protect Them.

As numerous studies have stated, concussions are mild traumatic injuries to the brain that result in swelling leading to further issues. So, being the sports crazed nation we are, how do we prevent brain injuries from occurring as well as taking the further precautions once they have happened? For starters, there have been a great deal of advancements from many equipment companies throughout sports that have been working to produce a helmet that both provides better protection as well as signaling when this protection was not quite enough to completely prevent someone from receiving a concussion.

From a hockey player’s prospective, I began skating before I was five years old and have gone from the Cooper helmets that were from the early nineties that offer about as much protection as if someone was to wear a 5-quart ice cream bucket on their head to wearing some of the newer brands like the recently bought out cascade helmets that were designed with concussion protection capabilities. Some companies are even beginning to work on placing sensors in helmets that detect the impacts taken during games and can signal when the impacts are reaching a severity that will require attention. How these work is they use a sensor that tracks both linear and rotational acceleration of the impacts and uses its signaling capabilities to transfer this data to a mobile app to keep record of the impacts taken during practices or games. The major piece being paid attention to is the rotational acceleration as that is the common factor in impacts that plays the greatest role in injuring the brain. During an impact that involves linear acceleration and no rotational acceleration, the brain is shifted in a front, back, or side-to-side fashion which is of course bad for the brain. At the same time these injuries have not been found to be as damaging the injuries that involve a bit of rotational acceleration as the impacts add another element to the brain injury. The rotational accelerations add a sheering force to the injury that causes not only a greater amount of damage but the twisting motion results in an overall faster, more forceful shifting of the brain resulting in more extensive injury.

Another attempt by companies to combat severe brain injury has been developed in the extreme sports market with a technology called MIPS or Multi-Directional Injury Protection System. MIPS has been an impressive advancement for brain protection as it works to protect from the extensive rotational acceleration injuries in athletes. This technology works by placing a layer that is fairly conforming to the top of the head as many helmets are designed to, but this thin layer is made from a material that has a very low friction coefficient allowing it to slide when a helmet receives an impact. By providing a sliding layer of protection, the brain has more defense against rotational acceleration as an impact occurs the outer shell may rotate as it hits the ground, but the MIPS layer will continue its normal trajectory thus preventing or lessening the added rotational element added to the impact.

These protective measures against concussions are not perfect but they are a good step in the right direction. It is important to continue the push for better technology to protect the heads of athletes especially children that have a great drive to be better athletes but do not understand the long-term consequences of brain injuries. Hopefully, in the future these advancements will keep getting more and more protective so parents don’t have to worry so much about the choice of whether it is a good idea to allow their child to participate in contact sports.
Fear, Anxiety, and the HPA Axis
To begin it must be made evident that Fear and Anxiety are in a sense necessary. We as humans thrive as a species because we have this innate response to fearful experiences. Our fears are responsible for activating the Hypothalamic-Pituitary-Axis (HPA) to elicit a stress response. This stress response allows our bodies to meet the needs of the stressful system to survive. The sympathetic response accounts for the adrenaline-like feeling we experience that can be described by elevated heartrate, respiratory rate, dilated pupils, and several other visceral responses. Most often, these responses are successful in helping us in acute fear eliciting instances.

The issue arises from the constant state of a fearful response which derives from anxiety. Anxiety is the state of worry that we might encounter our fears throughout our normal day of life. In some respects, this is a very helpful tool because it aids in keeping us alert when we are performing stressful tasks such as driving in the winter. The problem comes when our minds hold on to the anxious state during times that we should be in a parasympathetic state, or rest and digest as many might say. Many soldiers that come home from war experience this constant state of anxiety or in other diagnostic terms, post-traumatic stress disorder (PTSD).

PTSD is a common unfortunate burden soldiers bring home from wars that without proper coping or diagnosis can lead to severe issues. The problem in many cases of PTSD is the sudden sounds that elicit trained responses in these men and women causing them to act as they may have been trained to be prepared for combat. Furthermore, this issue leads them to further disorder such as chronic stress and depression.

Anxiety for most can be treated using several different methods, behavioral as well as pharmaceutical. Most commonly benzodiazepines are used as a treatment method for anxiety because it acts as an inhibitor of the system that activates sympathetic responses, leaving a more relaxed feeling instead of a stressful one.

Paired with anxiety that makes it such a harsh disorder is the fact that anxiety plays a huge role in memory formation. Being that fear is an innate trait we all have keeping us prepared for a stressful situation, we rely on memory to aid in recognizing dangerous situations. Long term potentiations play a dire role in memory formation due to the fact that they increase the ease of communication between our neuronal synapses especially in the hippocampus where we store our memories. The issue comes into play as we are not able to turn off these memories when we feel that they are causing great anxiety when a restful state is what should be called for. This is the ultimate unfortunate fact that those with great anxiety face as there is no cure for overactive memories especially those that cause us the greatest distress. Thankfully, behavioral therapy as well as mindfulness can help us cope with this burden as we attempt to carry on with normal day to day tasks.
Click This! Click This! Click This! and Learn About Addiction

Drug addiction is a hot topic of late, both with regards to scientific understanding and social action. The United States has been ramping up border protection in an effort to mitigate drug usage, and Portugal has legalized all drugs for recreational use in hopes of improving public health by de-stigmatizing drug addiction.
The question at the forefront of this issue is whether or not it is within our power to break away from our addictions.
Tackling this issue becomes difficult for several reasons. From a social standpoint, our society has been deeply influenced by Cartesianism ( https://en.wikipedia.org/wiki/Cartesianism ), and we think that our mind has the power to overcome every and all obstacles with sheer determination. The glorification of the mind over body mentality continues today with movies depicting soldiers and athletes overcoming their respective pain and achieving the goal they set out to achieve.
This is all fine and dandy, but it minimizes the power of the brain, and I believe it is the root of stigmatism in the U.S.
So what is happening in a person’s brain who’s struggling with addiction? For starters, addict’s “reward centers” in the brain are being overwhelmed. Our brains help us out by making us feel good whenever we do something that’s supposed to be good for ourselves. One example of this is eating some ice cream. Our brain processes the  signal from our mouth, and tells us “Ice cream good, eat more.” So we eat more because it feels good.This feeling good comes from a place in the brain called the Striatum (marked in green on the picture below). Our Striatum releases a neurotransmitter called dopamine, and we receive a feeling of pleasure.
signal from our mouth, and tells us “Ice cream good, eat more.” So we eat more because it feels good.This feeling good comes from a place in the brain called the Striatum (marked in green on the picture below). Our Striatum releases a neurotransmitter called dopamine, and we receive a feeling of pleasure.
Drugs:
So where do drugs fit into all of this? Particularly addictive drugs like methamphetamine and heroin hijack your Striatum. These drugs cause a huge amount of dopamine to be dumped into your brain and cause a feeling of intense pleasure and euphoria. Herein lies the problem with drug addiction. The Striatum’s job is to promote continued action by making us feel good. When we stimulate that region of our brain with an action, such as taking some prescription pills or illegal substances, our brain becomes hardwired to wanting to repeat that action. The dial gets turned up to 11 when we do this with addictive drugs because of the amount of dopamine released. Several proteins and cellular pathways become activated in our brain to rewire it. Some of the proteins such as protein kinase A and C serve to cause cellular restructure and proliferation.
When we take all that’s happening to our brains into account, we see that drug addiction becomes less and less of a choice and more of necessity. Our brains become trained to want drugs more than things like life-sustaining food. It seems confusing that our brains would rather have drugs and die instead of being healthy. But that’s because living healthy doesn’t always activate our striatum. Simply put, our brain gets turned against us when addictive drugs are put into the equation. We become erratic and irrational.
Regardless of your stance on drug addiction, please let anyone you know struggling with addiction that there are people out there who are willing to help them without any judgement. The hotline for drug abuse is 1-877-978-2486, and you can find there website here http://drugabuse.com
Recapping the Capstone
Neurochemistry sounds kind of scary, doesn’t it? Well let me tell you that it was a great class. The structure and organization of the class created a great environment for all the students to have interesting dialogues. We learned about a neurological disease every week from a scientific literature standpoint. By doing this we discussed the paper in full, researched new topics relating to the disease, and had open dialogue to discuss the disease. This has been one of my favorite classes at Concordia College and any upcoming senior should definitely consider taking it. Mental health diseases affect so many people around the world and so many of our friend and family either know someone affected or are affected. By taking this class you can further your knowledge on these topics and develop an understanding and compassion for people that suffer from these diseases.
We also were required to do a community action project where we had the opportunity to spread awareness of a disease of choice. This was a great project that I had a lot of fun taking my time and effort to actually do something concerning a disease. I will miss the weekly couch dialogues every Friday and listening to everyone’s opinions. Thank you Dr. Mach for a wonderful experience!
It Is Time to Think Differently
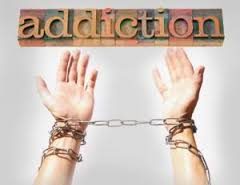
What do you think when you hear the word “addiction”? Do you think that it’s a choice? Do you stigmatize people who are claimed to suffer from the word “addiction”? What if I told you that addiction is a disease? What would you say? Well….. I’m here to argue that addiction is a biological disease.
First lets define what addiction is.
The International Statistical Classifications of diseases and Related Health Problems (ICD-10) defines addiction, characterized as uncontrollable and unpleasant mood states leading to compulsive drug seeking behaviors and taking the drug despite negative consequences. The ICD-10 is a criterion for diagnosing diseases that was created by physicians, psychiatrists and psychologists. A disease is defined by “a disorder of structure or function in a human, animal, or plant, especially one that produces specific signs or symptoms or that affects a specific location and is not simply a direct result of physical injury.” What I hope to do now is explain why addiction fits into the general definition of a disease.
A review article in the Frontiers of Neuroanatomy journal explains how addiction affects the striatum, (which is an area in your brain) as well as the signal transduction in your brain that is responsible for not only cell activity but also for how you think, feel, and behave. Addictive substances bind to receptors in your brain which then releases neurotransmitters such as glutamate and dopamine and carry out their effects in this way. The striatum is an important area when researching and discussing addiction as this area of the brain contains the Nucleus Accumbens (NAc) and the Ventral Tegumental Area (VTA), which are involved in the mesolimbic reward system.

The brain reward system is responsible for making you feel good or a reward from a certain stimulus. Drugs of abuse target this natural biological mechanism and hijack it to manipulate the individual to form stronger memories that are related to drug seeking behavior.
.
Drugs can induce proteins to be created to change and strengthen neuronal connections within the brain that favor maladaptive behavior. Chronic Drug Abuse is characterized with the built up of pharmacological tolerance, dependence and sensitization. Tolerance is characterized as needing more of the drug to experience the same “reward”. Dependence is characterized as experiencing withdrawal symptoms if the intake of the drug stops. Sensitization is the experience of the individual to crave the drug. The reason why these aspects occur is because receptors in your brain change their composition in number because there is so much neurotransmitter readily available that your body does not need as many receptors. So once drug intake ceases there is not enough neurotransmission occurring because there is a decreased amount of receptors and this is when the individual experiences withdrawal symptoms. Withdrawal symptoms vary by drug specificity but some examples are sweating, headaches, tremors, nausea, irritability, etc. People can overcome addiction by completely abstaining from the substance but are at high risk for relapse for many years after.
So, I think I have established a specific structure in the human body that is dysfunctioning and as a result the individual experiences withdrawal symptoms and compulsive drug seeking behavior that is unavoidable. Doesn’t this fit into the general definition of a disease? It’s weird to think that your brain is a part of your biological body. I’m not sure why people try to separate it. But anyways, the causes and risk factors for addiction exist in a broad spectrum. It could be due to social peer pressure, genetic predisposition, prescription drugs, dealing with a life hindrance, or taking drugs to escape other symptoms from comorbid mental illnesses.

Addiction affects around 20 million Americans and around 1 and 10 people suffer from the disease. Around 100 people die everyday from drug overdose in the United States and in 2015 drug overdose claimed the lives of over 50,000 people. Addiction doesn’t kill just by overdose deaths either; other factors such as accidents and suicides are a huge problem with the prognosis of addiction. It is time to change the way we view addiction as a society so that we can create progressive changes and stop these senseless deaths and crimes.
Pathways of Schizophrenia
I am a uniquely situated person. I am a biochemistry major with a sociology minor. At this point in time it puts me in both an introductory sociology class and my upper level chemistry course about the chemistry of the brain. This put me in an interesting position while discussing mental illness in sociology. The idea that mental health is dependent on how you were raised and what experiences you have is a problematic idea. Now that is not to say that how you were raised and your experiences do not shape mental illness but to say that you have your mental illness because of how you were raised is not okay. Take for example schizophrenia.
Schizophrenia is a mental disorder where individuals experience hallucinations or paranoia. These hallucinations can be seeing 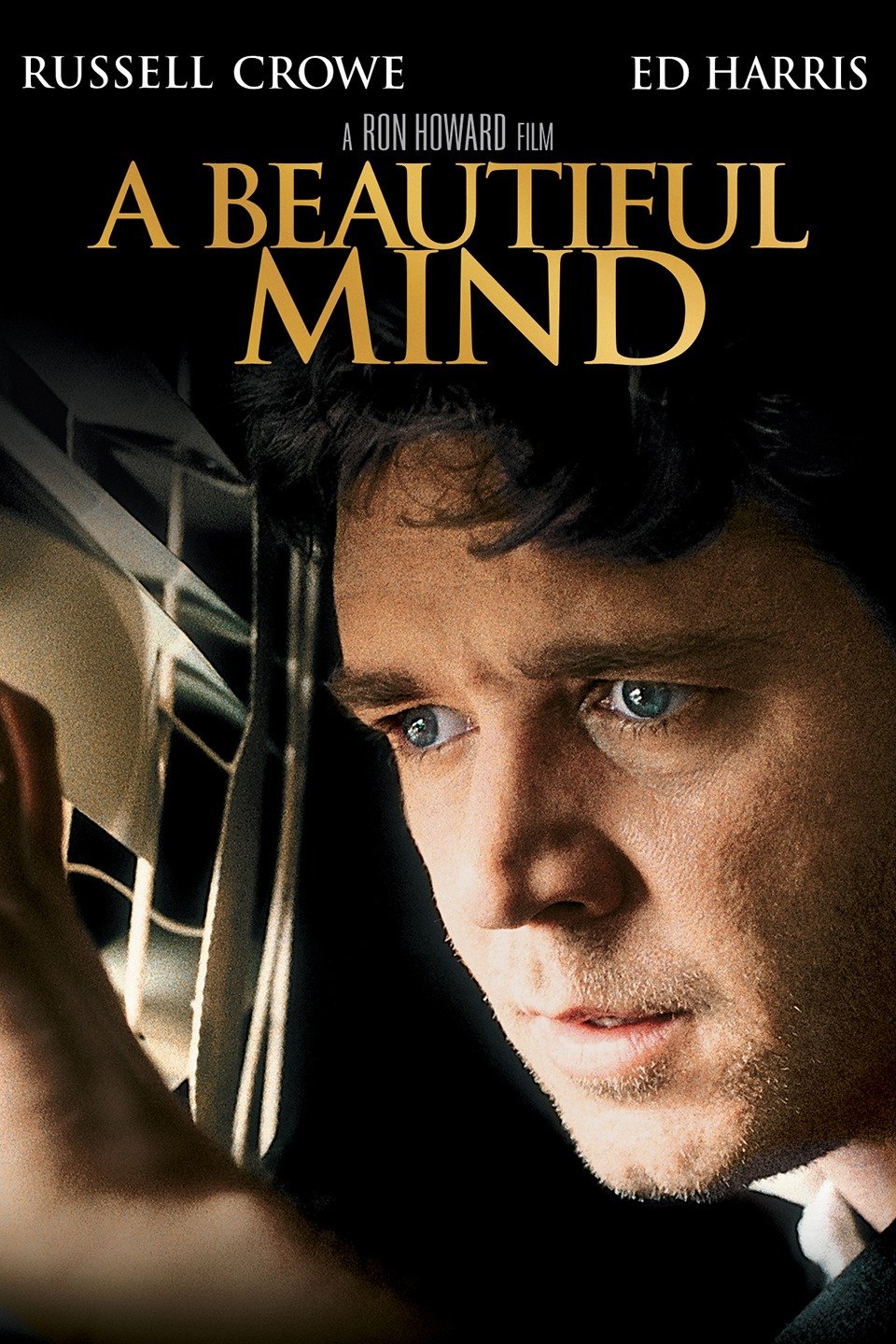 things that are not there, hearing things, and smelling things that are not there. Paranoia can be thinking that someone is trying to kill you or delusions of grandeur. One of the good examples of schizophrenia in the media is the movie “A Beautiful Mind”. The movie is about the journey of a very famous mathematician John Forbes Nash Jr. and how he experienced schizophrenia. One of the most saddening moments of the movie is when he is walking through the crowded campus yelling at his hallucinations. One of the greatest struggles with being diagnosed with schizophrenia is that patients then have to understand and accept that they way they see the world is not real.
things that are not there, hearing things, and smelling things that are not there. Paranoia can be thinking that someone is trying to kill you or delusions of grandeur. One of the good examples of schizophrenia in the media is the movie “A Beautiful Mind”. The movie is about the journey of a very famous mathematician John Forbes Nash Jr. and how he experienced schizophrenia. One of the most saddening moments of the movie is when he is walking through the crowded campus yelling at his hallucinations. One of the greatest struggles with being diagnosed with schizophrenia is that patients then have to understand and accept that they way they see the world is not real.
The reality of schizophrenia is it is not very common. According to the National Institute of Mental Health only approximately 1.1% of people in the United States have the disease. However that can range from mild to very severe cases. This can be a very hard thing for patients and their families to deal with. That is one of the reasons that looking at schizophrenia as if it is caused by how a person was raised is really problematic. Not only do individuals have to deal with the disease and all that is involved but then it is also their fault that they have it in the first place.
THIS IS NOT TRUE.
Schizophrenia is caused by chemistry in the brain. In particular neuroscience suggest that it is due to imbalances in the Wnt pathway. Pathways are what we call the rout that signals take from the outside of the cell to other parts of the cell. It is similar to a game of telephone. A receptor on the outside of the cell gets a signal it then tells a signaling molecule who tells another signaling molecule and the signal is sent to where it needs to go, in this case the nucleus. In the Wnt pathway, Wnt is the receptor that starts this molecular game of telephone. Now it should be said that molecules are specifically better at telephone than most human beings so there are more options for what the end of the telephone game will be. In the one pathway signals can be sent to the nucleus where genes are expressed or it can directly effect other parts of the cell. Also molecules are good at stopping pathways after the signal is sent to there is not too much information happening at once.
One of the biggest players in the Wnt pathway is GSK. GSK helps to send the molecule beta-catenin in to the nucleus to express genes that are necessary for the cell. What is proposed in schizophrenia is that GSK does this job to well and there is too much beta-catenin entering the nucleus. The extra beta-catenin causes over expression of memory genes and may cause the formation of signals that are not really there.
Schizophrenia is still not fully known and so more research should be done to understand how this pathway can be regulated but one thing is certain. It is not an individuals fault if they have schizophrenia and the best thing we can do for them is to help them understand that and make it easier to seek out treatment.