Cannabis is a plant that has been used for medicinal, recreational, and spiritual purposes for thousands of years. It contains over 100 active compounds known as cannabinoids, tetrahydrocannabinol (THC) and cannabidiol (CBD), which are the most well-known compounds and interact with the body’s endocannabinoid system to produce various physiological and psychological effects.
CBD vs THC
THC is psychoactive and produces a “high” when consumed, whereas CBD does not produce a high and is not intoxicating. THC is known for its pain-relieving properties and is often used to alleviate symptoms of conditions such as chronic pain, nausea, and glaucoma. CBD, on the other hand, has been shown to have anti-inflammatory, antipsychotic, and anti-anxiety effects, and is often used to alleviate symptoms of conditions such as anxiety, epilepsy, and insomnia. Both CBD and THC can have side effects, such as dry mouth, dizziness, and fatigue, but they are generally considered safe when consumed in moderation [1].
History of Cannabis
Cannabis has been used by humans for thousands of years for medicinal, spiritual, and recreational purposes. It is believed to have originated in Central Asia and spread throughout the world through trade and migration.
Ancient civilizations such as the Chinese, Egyptians, and Greeks used cannabis for various purposes, including pain relief, anxiety, and religious ceremonies. In the 19th century, cannabis was widely used in Western medicine, but its popularity declined with the advent of synthetic drugs.
In the 20th century, cannabis was criminalized in many countries due to its association with drug abuse and social unrest. However, in recent years, there has been a growing movement towards legalization and acceptance of cannabis for both medicinal and recreational use [2].
Alcohol vs Cannabis and the Human Brain
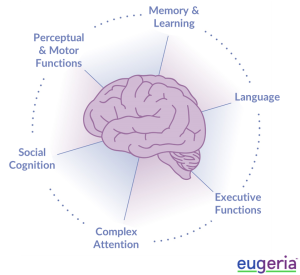
Both alcohol and cannabis can affect the human brain in different ways. Alcohol is a central nervous system depressant that can impair cognitive and motor functions, leading to impaired judgment, slowed reaction times, and decreased inhibitions. Chronic alcohol abuse can also cause brain damage and increase the risk of neurological disorders such as dementia and Alzheimer’s disease.
In contrast, cannabis contains compounds called cannabinoids, which can have both psychoactive and therapeutic effects. THC, the main psychoactive component in cannabis, can cause short-term memory impairment, altered perception of time, and impaired coordination. However, cannabinoids have also been shown to have potential therapeutic benefits for conditions such as chronic pain, anxiety, and epilepsy. Overall, more research is needed to fully understand the effects of alcohol and cannabis on the human brain [3].
Long-term Exposure to Cannabis
Long-term exposure to cannabis can have negative effects on a person’s physical and mental health. Chronic use of cannabis can lead to respiratory problems, such as chronic bronchitis and lung cancer, as well as cardiovascular problems, such as increased heart rate and blood pressure.
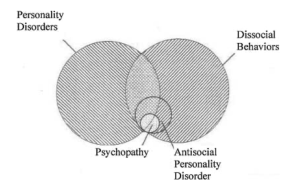
Cannabis use can lead to dependency, which is characterized by compulsive drug-seeking behavior and withdrawal symptoms upon cessation of use. While cannabis dependency is less severe than addiction to other drugs, it can still have negative impacts on an individual’s life and health. Research suggests that around 9% of cannabis users develop a dependency, and this risk is higher for those who begin using at a young age or use frequently. Additionally, the potency and method of use (such as smoking versus edibles) can also affect the risk of developing a dependency. It is important to monitor one’s cannabis use and seek help if dependency is suspected.
Additionally, long-term cannabis use can lead to the development of cannabis dependency, which can cause withdrawal symptoms such as irritability, insomnia, and decreased appetite. However, it is important to note that not everyone who uses cannabis will develop dependency, and the risk of dependency can be influenced by various factors, including genetics and environmental factors [4].
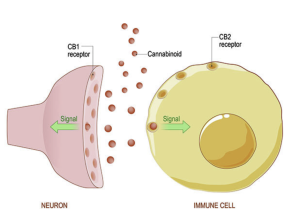
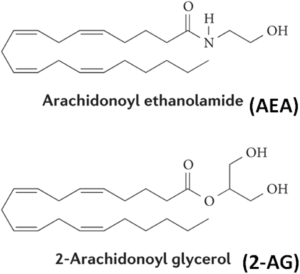
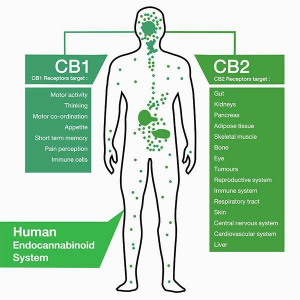
CB1 and CB2
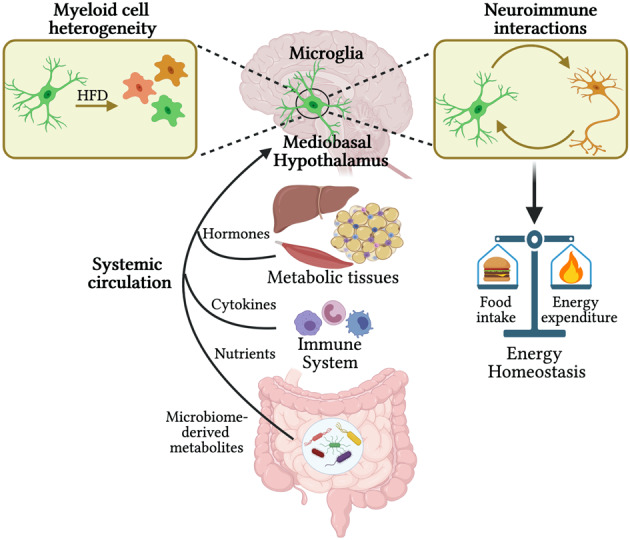
CB1 and CB2 are two receptors in the human body that are part of the endocannabinoid system. CB1 receptors are primarily found in the brain and central nervous system, while CB2 receptors are mainly found in the immune system and peripheral tissues. When cannabis is consumed, its active compounds, such as THC, bind to these receptors, leading to various physiological and psychological effects. THC primarily binds to CB1 receptors, which can lead to euphoria, relaxation, and altered perception. CBD, another active compound in cannabis, does not directly bind to these receptors but can modulate their activity and influence the effects of THC. Understanding the role of CB1 and CB2 receptors in cannabis effects is important for developing targeted therapies and minimizing adverse effects.
The endocannabinoid system (ECS) is a complex signaling network that is present throughout the body, including the central nervous system (CNS). The ECS is comprised of endocannabinoids, receptors, and enzymes that work together to regulate various physiological processes, such as mood, appetite, pain sensation, and memory. In the CNS, the ECS plays a critical role in regulating neuronal activity and neurotransmitter release, helping to maintain homeostasis and support proper brain function. The two main types of ECS receptors, CB1 and CB2, are expressed in the CNS, with CB1 being particularly abundant in the brain. Activation of CB1 receptors can modulate neuronal excitability and neurotransmitter release, and dysregulation of the ECS has been implicated in various neurological disorders [5].
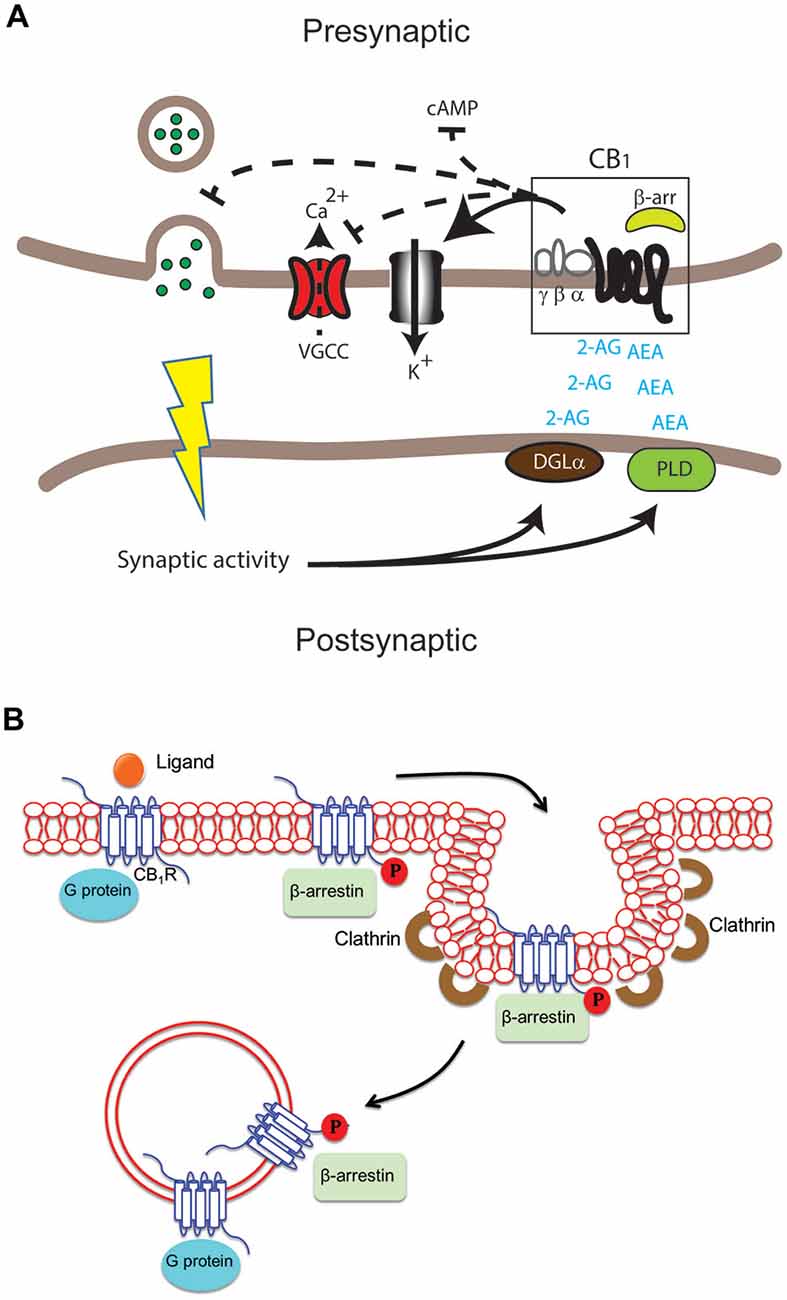
Figure 1. Cannabinoid Receptors Signaling
Resources
[1] MediLexicon International. (n.d.). CBD vs. THC: Differences, benefits, and effects. Medical News Today. Retrieved May 1, 2023, from https://www.medicalnewstoday.com/articles/325871#legality
[2] Crocq, M.-A. (2020, September). History of cannabis and the endocannabinoid system . Dialogues in clinical neuroscience. Retrieved May 1, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7605027/
[3] Noorbakhsh, S., Afzali, M. H., Boers, E., & Conrod, P. J. (2020, March 2). Cognitive function impairments linked to alcohol and cannabis use during adolescence: A study of gender differences. Frontiers. Retrieved May 1, 2023, from https://www.frontiersin.org/articles/10.3389/fnhum.2020.00095/full
[4] U.S. Department of Health and Human Services. (2023, April 17). What are marijuana’s long-term effects on the brain?National Institutes of Health. Retrieved May 1, 2023, from https://nida.nih.gov/publications/research-reports/marijuana/what-are-marijuanas-long-term-effects-brain
[5] Kendall, D. A., & Yudowski, G. A. (2017). Cannabinoid receptors in the central nervous system: Their signaling and roles in disease. Frontiers in Cellular Neuroscience, 10. https://doi.org/10.3389/fncel.2016.00294




 Artstract on DALL.E
Artstract on DALL.E