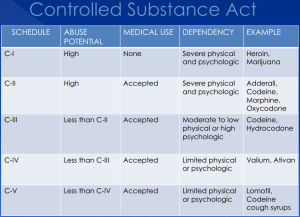
When people hear anything about the endocannabinoid system their minds often go right to thinking about marijuana. Which isn’t surprising as marijuana use is increasing. According to the National Council of State Legislature, as of now 38 states in the US has approved medical marijuana use. It is not often that you get to see such a mass use, and approval of a schedule 1 class substance. In my opinion in all seems like it should be and is a touch and go process. With marijuana being a schedule 1 substance it very hard to study. There is very limited amount facilities able to study it and then limitations on the type of studies that are able to be done.
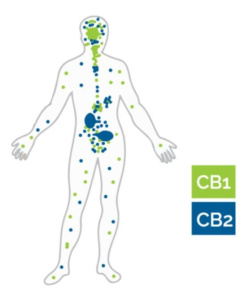
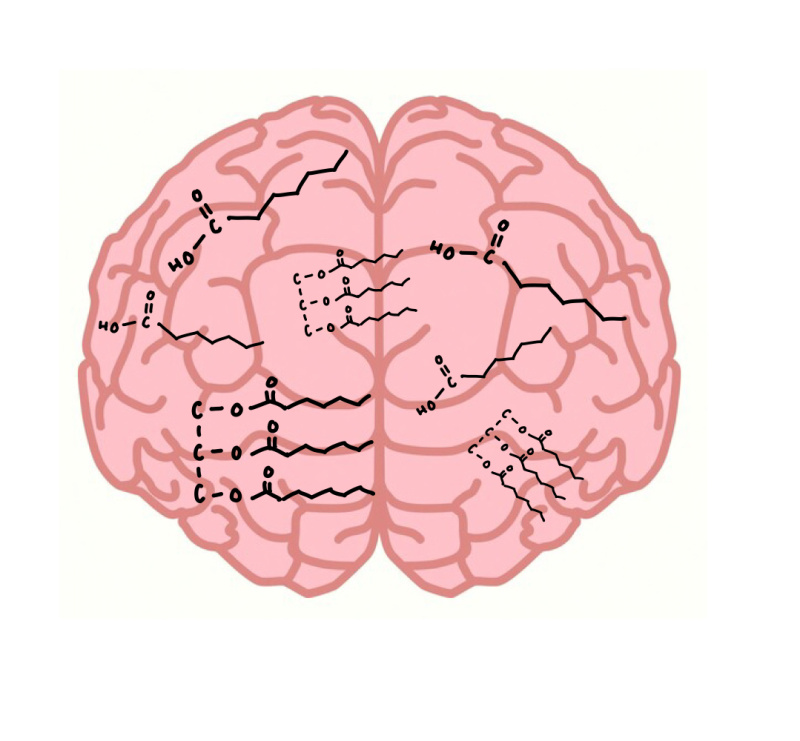
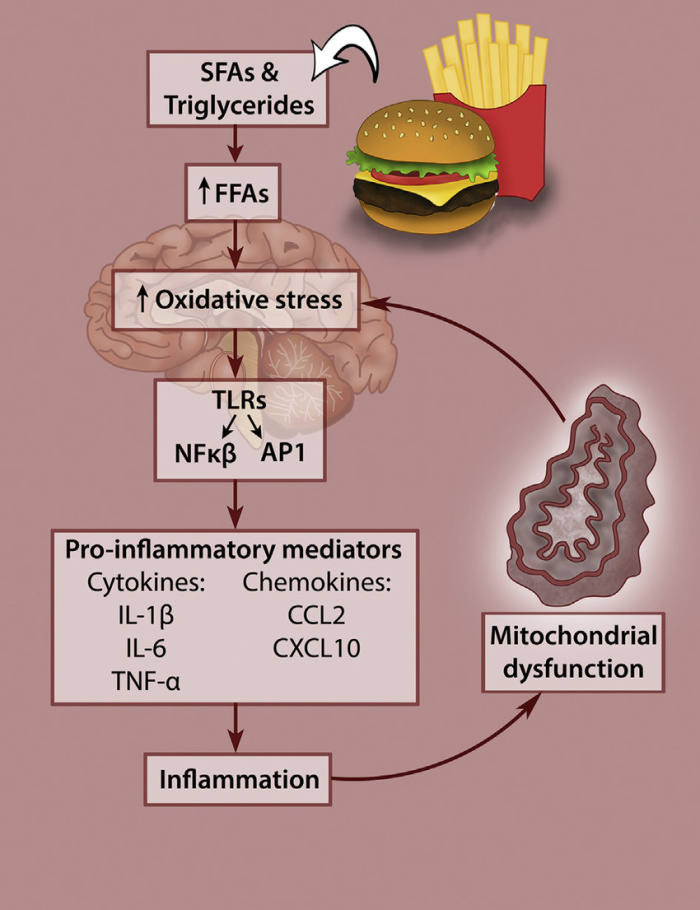
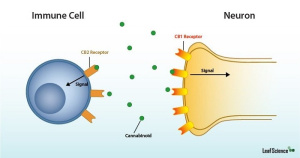
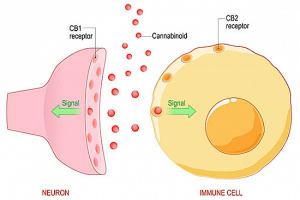
In 2019 the CDC reported that 18% of Americans had used marijuana that year. This is both medically and recreationally. The basis of marijuana’s effects on the endocannabinoid system is pretty mapped out. Yet, red flags do pop up for long term effects, effects on other system, etc. G protein coupled receptors (GPCRs) are the causes the activation of endocannabinoid system. One of the most common note mentioned about activating endocannabinoid system (mostly by marijuana use) for treatment is the widespread effects, expression and many complex cascades that happen.
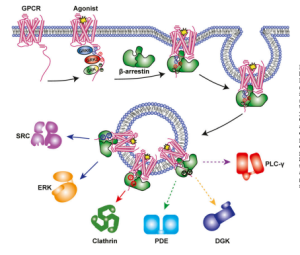
 The barcode hypothesis is often brought up. A unique characteristic about GPCRs is that phosphorylation occurs and that determines their roles downstream. It also gives the guide for how or which beta arrestin binds to the GPCR. Phosphorylation can cause the GPCR to be inhibited, it can cause activation of other membrane receptors, one article 2017 even mentions that a certain pattern can cause the GCPR’s to detach from the membrane. That is where the term barcode hypothesis comes from.
The barcode hypothesis is often brought up. A unique characteristic about GPCRs is that phosphorylation occurs and that determines their roles downstream. It also gives the guide for how or which beta arrestin binds to the GPCR. Phosphorylation can cause the GPCR to be inhibited, it can cause activation of other membrane receptors, one article 2017 even mentions that a certain pattern can cause the GCPR’s to detach from the membrane. That is where the term barcode hypothesis comes from.
Yet, now think other than the phosphorylation pattern there is no control on the role that the GCPR is going to take. That certain barcodes cause certain cascades to occur causing a mass range of possibilities of expression.
Another article goes in to great detail cataloging all the different kinases and beta arrestins that can bind to GPCRs in the Endocannabinoid system. They also looked at the downstream effects that they had on the GPCR pathway. Phosphorylation effects if it binds on its side or in the middle. Even the affinity of the binding was all looked at. They found that the pattern of the phosphorylation mattered more than that number of phosphates. Which if you have been in the biochemistry world, you know structure equals function. Certain binding would even cause a conformational change for either the whole arrestin, but also only parts of the arrestin. This can directly effect binding of proteins downstream to the tail of the arrestin.
Why would this matter?
Well as mentioned earlier, studying the endocannabinoid system in regarding to marijuana’s effects is very hard. Yet it is legally allowed to be used and instructed as a treatment. Yet the truth is, it may cause benefits especially in the short term, but what about the long term? In my opinion makes me wonder why research restrictions couldn’t be lifted. That there are great possibilities that could from targeting the endocannabinoid system, but more precision would be nice to cut out any possible risks.

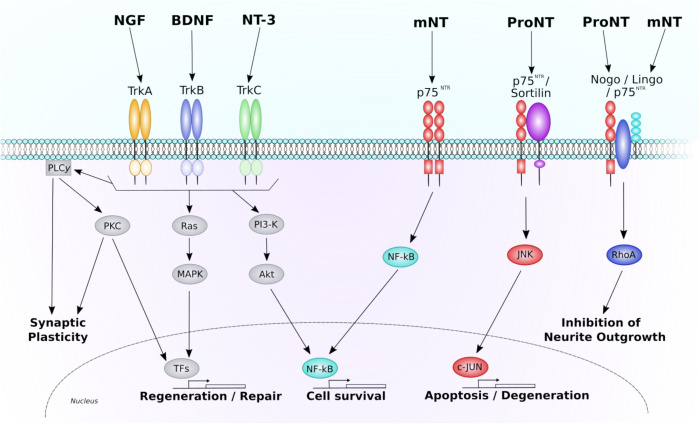
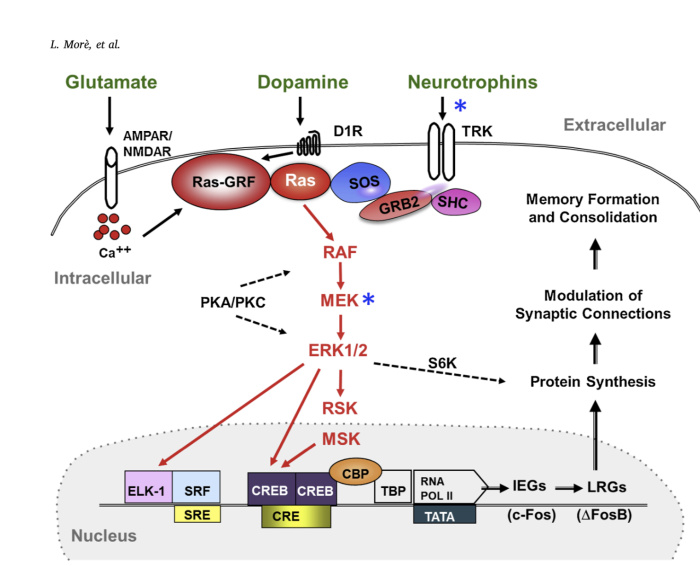

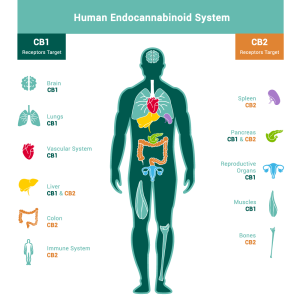
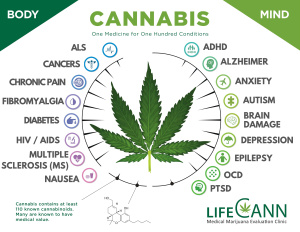

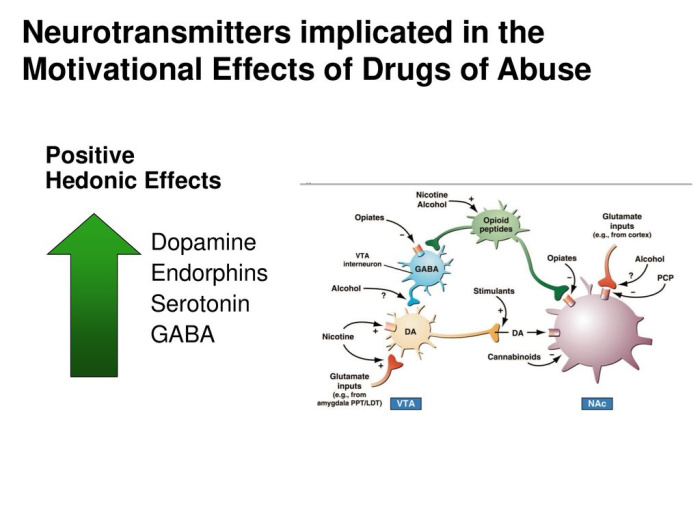
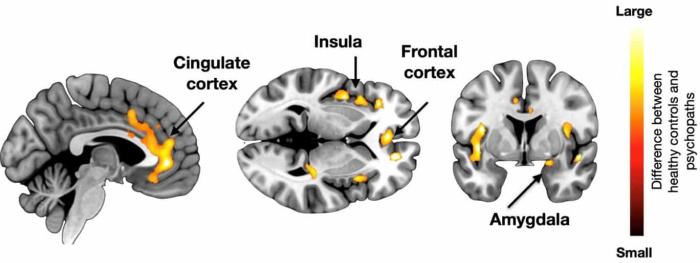
 Now that we know what the key players are, what exactly is the endocannabinoid system used for? The endocannabinoid system (ECS) has emerged as one of the key regulatory mechanisms in the brain that controls many events such as mood, pain, perception, learning, and memory. It may also provide a neuroprotective role in brain injury as well as potentially playing a role in drug abuse and dependence.
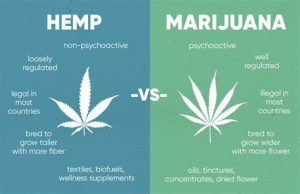
Now that we know what the key players are, what exactly is the endocannabinoid system used for? The endocannabinoid system (ECS) has emerged as one of the key regulatory mechanisms in the brain that controls many events such as mood, pain, perception, learning, and memory. It may also provide a neuroprotective role in brain injury as well as potentially playing a role in drug abuse and dependence.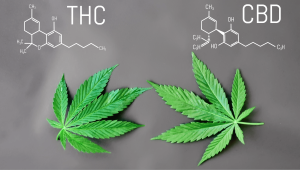 Let’s talk drugs, such as cannabis (better known as marijuana, pot, weed, grass, dope). Cannabis is a psychoactive drug from the actual cannabis plant. There are two main components of the cannabis plant.
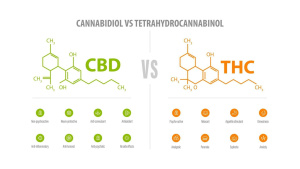
Let’s talk drugs, such as cannabis (better known as marijuana, pot, weed, grass, dope). Cannabis is a psychoactive drug from the actual cannabis plant. There are two main components of the cannabis plant.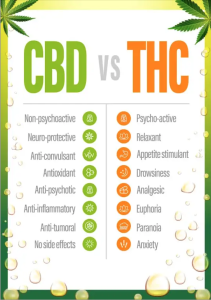 One major difference between these two is that CBD is legal in all 50 states whereas THC is only legal (or decriminalized) in 22 states. There are also more forms of CBD than that of THC.
One major difference between these two is that CBD is legal in all 50 states whereas THC is only legal (or decriminalized) in 22 states. There are also more forms of CBD than that of THC. It can be seen that white people and people of color are using marijuana at the same rate, but people of color (specifically African Americans) are arrested for violating marijuana possession laws at nearly
It can be seen that white people and people of color are using marijuana at the same rate, but people of color (specifically African Americans) are arrested for violating marijuana possession laws at nearly 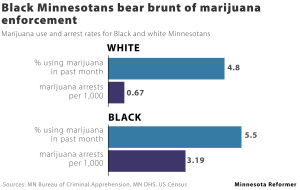
 While CBD is legal in 50 states there are still interesting statistics that can be talked about! Roughly
While CBD is legal in 50 states there are still interesting statistics that can be talked about! Roughly