Marijuana Usage in the USA is Increasing
A recent Gallop poll found 49% (up from 45% in 2017) of Americans have tried marijuana in some form at some point (Hubbard, 2021). Some are doing it for health benefits, others for recreation. Whatever reason people are using marijuana, it is clearly an important topic to discuss based on the sheer amount of people using it in the USA alone. To learn more about the stats and history of marijuana in the US, check out this link! There are some interesting health benefits to some of the compounds in marijuana called cannabinoids. The two most well known and studied are THC and CBD. At this point in time, these chemical abbreviations are nearly household names! In this post, we will explore some of the health benefits of CBD and THC are, as well as explaining the science behind why these chemicals can be so effective.
Is Cannabis Really “Naturally” Found in the Brain?
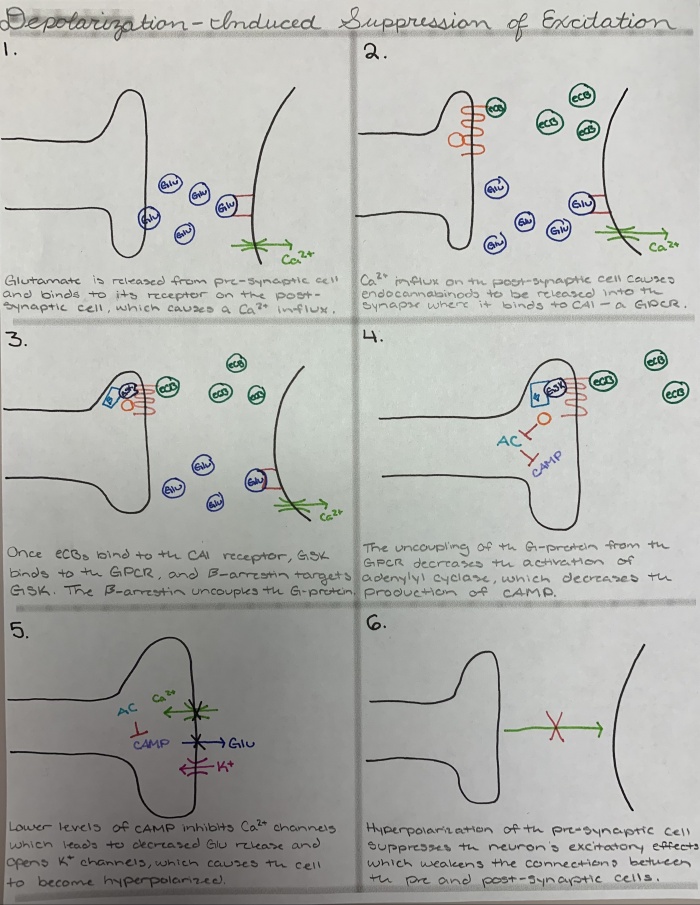
Yes. No. Well, sort of! The brain produces a class of chemicals called endocannabinoids. these have names like anandamide, arachidonylethanolamine, and 2-archidonoyl glyerol. These are endogenous cannabinoids, similar to form and function to THC and CBD. Fun fact, anandamide is derived from the Sanskrit word “ananda” which means internal bliss (Scherma, 2019). The Sanskrit meaning hints at some of its functions in modulating brain chemistry.
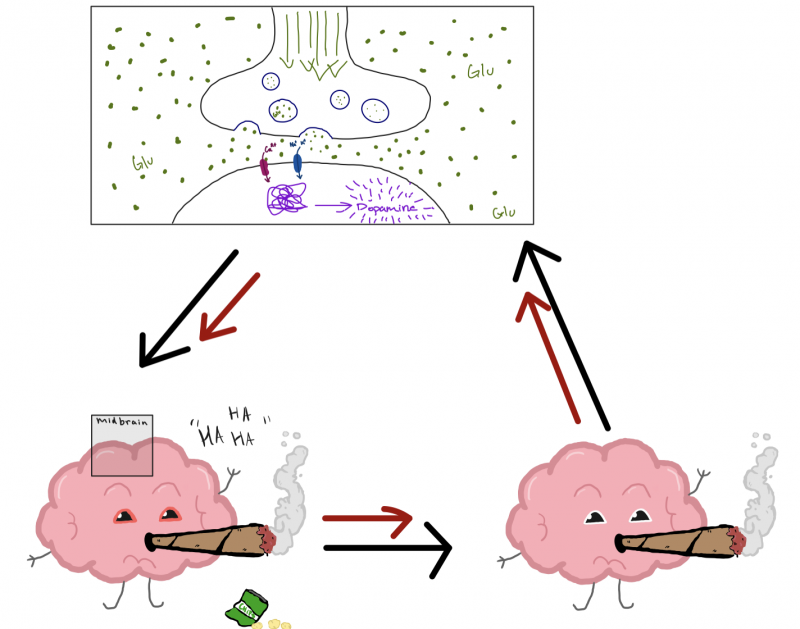
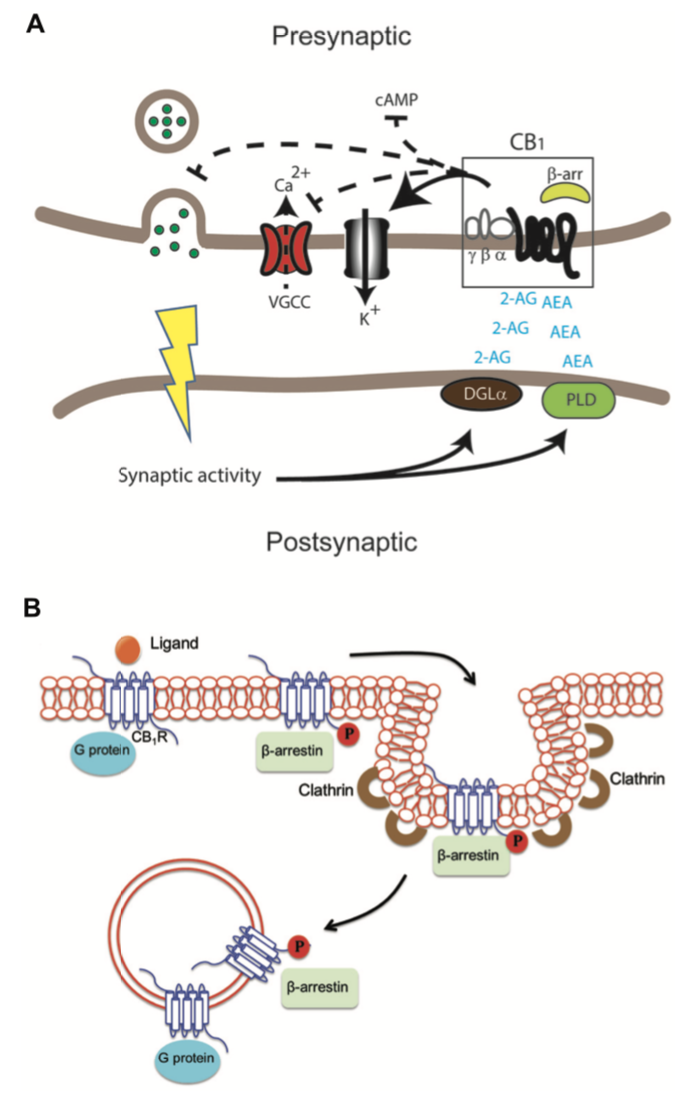
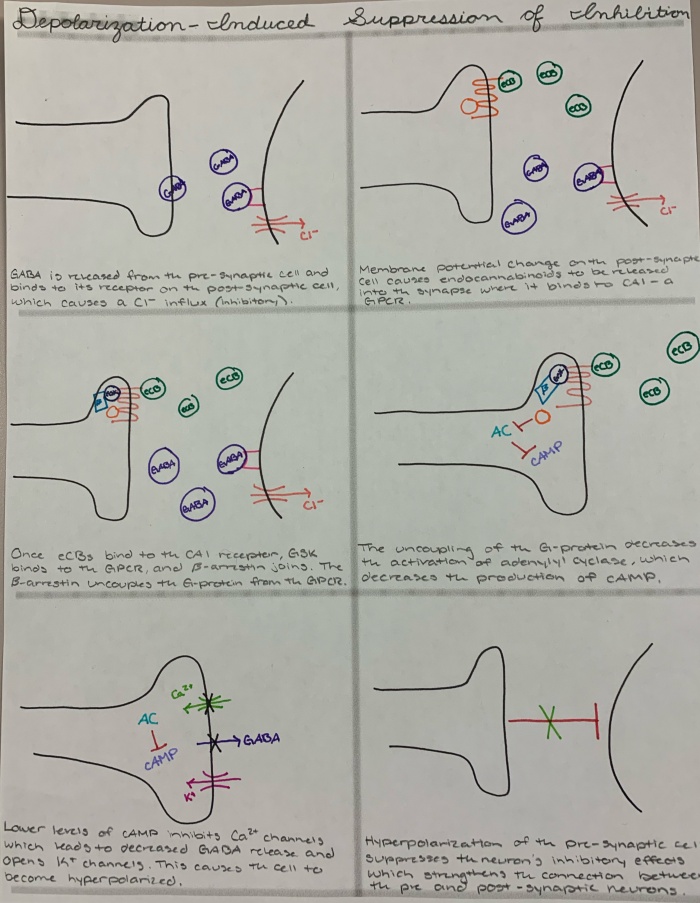
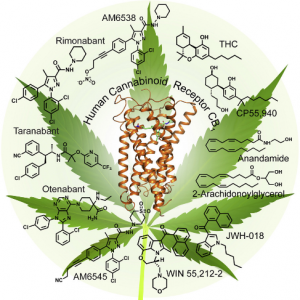
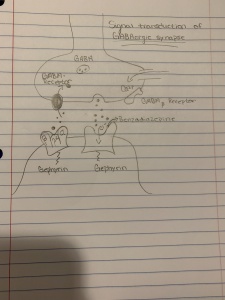
Interesting! But where do these endocannabinoids come from? Interestingly, they are modified from fat in your cell membranes. Neuronally, this occurs in the post-synaptic neuron, AKA the neuron being being stimulated. See figure 1 below for a nice visual.
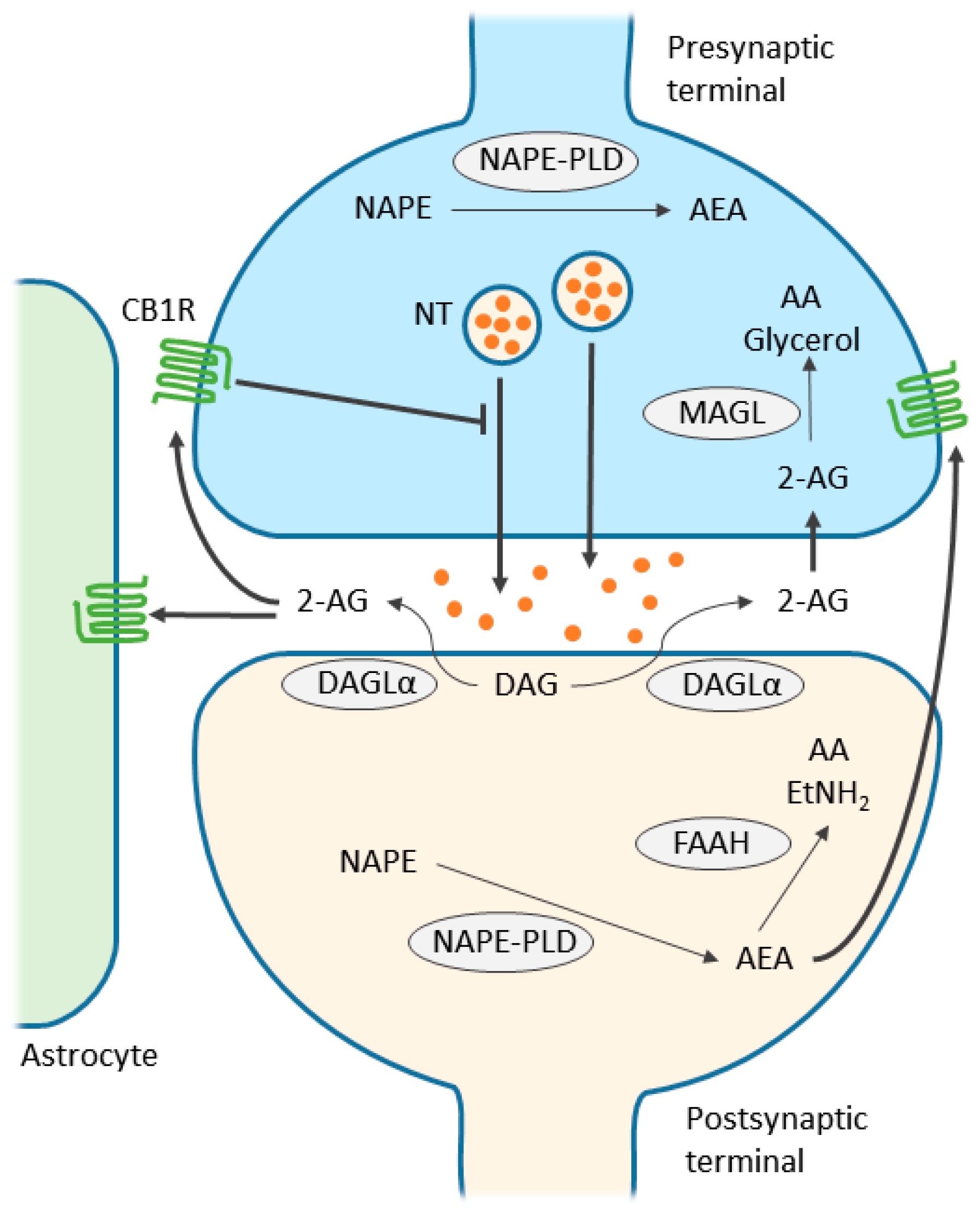
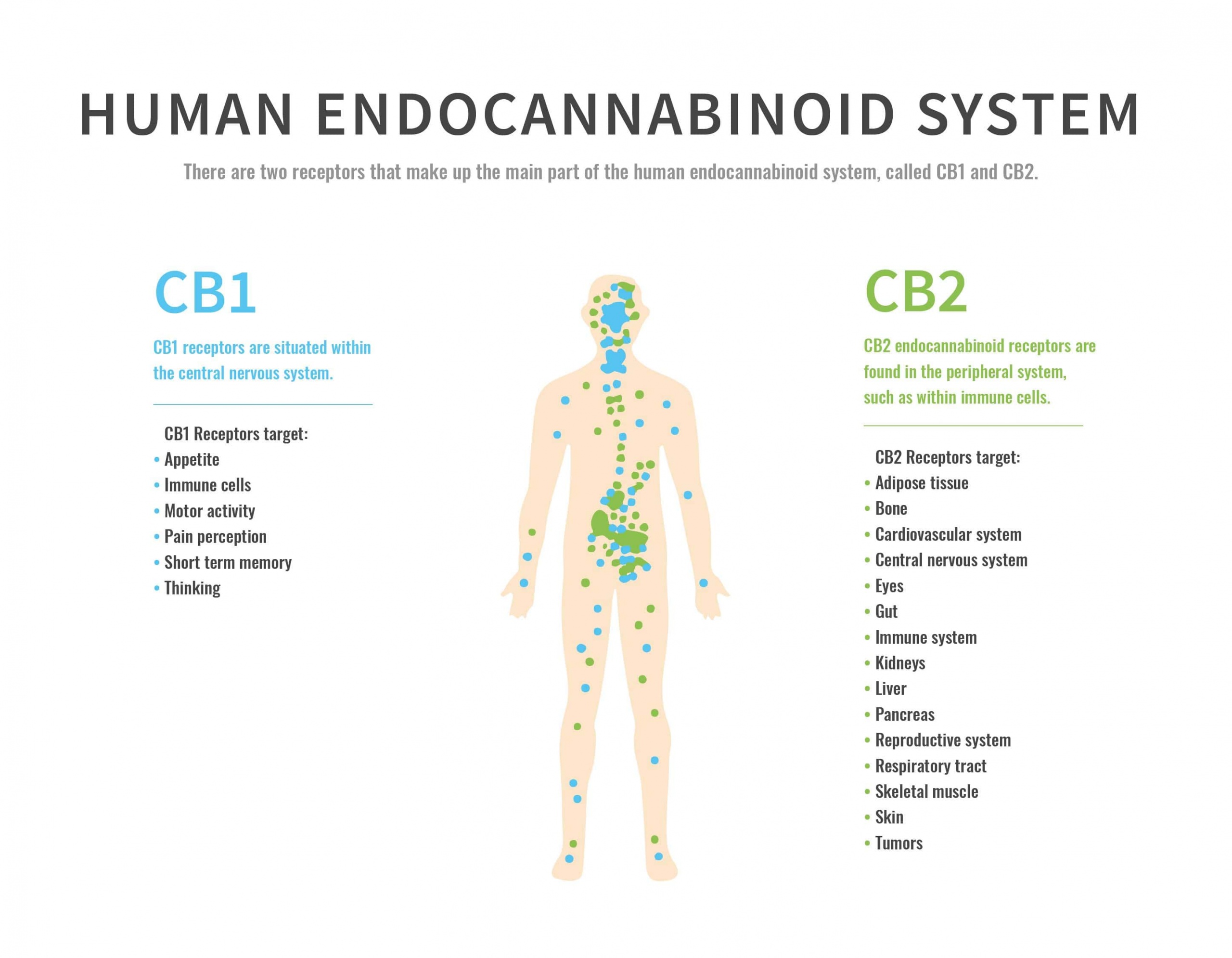
So great. We know the names of several endocannabinoids, but they have to bind somewhere to exert any of their effects. Endocannabinoids bind primarily to two receptors: CB1 and CB2 (Kendall, 2017). CB2 receptors are mostly found in the immune system, and when activated by endocannabinoids, inflammation levels increase and drug self-administration frequency decreases (Kendall, 2017). On the other hand, CB1 receptors are expressed throughout the body (Kendall, 2017) and are responsible for many of the positive benefits and side effects of THC and CBD.
Health Benefits of THC and CBD
The claims made online about what THC and CBD can do to a person range anywhere from giving one brain damage, to curing any ailment. Unfortunately, because because marijuana is a schedule I drug, conducting research on it is very difficult and makes a lot of these claims unsubstantiated. Because of this, I will focus on only a few of the positives of cannabinoids that I feel are substantiated with at least some rigorous, scientific evidence.
Should Grandpa Be Toking Up?
An interesting study conducted in mice found that older mice given THC had improved memory (Sarne, 2018). Not only did these old THC mice have the memories that matched young mice, but so did the expression levels of genes involved with memory (Sarne, 2018). This suggests that THC administration could be a viable way to slow or even reverse aspects of aging in the brain (Sarne, 2018).
What About CBD?
When one reviews the literature on CBD, it becomes apparent that it’s anti-inflammatory properties are one of it’s greatest assets in treating disease. A randomized clinical trial (RCT) found CBD is effective at significantly reducing the pain caused by arthritis (Verrico, 2020). Another study found that CBD can help treat Chron’s disease, and even wean some people off of steroid therapy (Naftali, 2013). Yet another RCT found CBD to be effective in preventing inflammation driven hyperpermeability of the human gut (Couch, 2019). The connection between all these studies is the anti-inflammatory effect of CBD. Too much inflammation can lead to many different diseases, and CBD seems like an effective tool to combat excess inflammation.
Conclusion
The amount of Americans using marijuana has been increasing ever since the records began. Because it is a schedule 1 drug, research using marijuana is very difficult and there are many questions science can answer, but isn’t being allowed to do so. Nonetheless, some promising studies have been conducted and have found health benefits for both THC and CBD. From the memory enhancing and anti-aging effects of THC, to the anti-inflammatory benefits of CBD, cannabinoids offer hope for treating a variety of ailments.
Sources
Couch, D. G., Cook, H., Ortori, C., Barrett, D., Lund, J. N., & O’Sullivan, S. E. (2019). Palmitoylethanolamide and Cannabidiol Prevent Inflammation-induced Hyperpermeability of the Human Gut In Vitro and In Vivo-A Randomized, Placebo-controlled, Double-blind Controlled Trial. Inflammatory bowel diseases, 25(6), 1006–1018. https://doi.org/10.1093/ibd/izz017
Hubbard, K. (2021). Record high: More Americans are trying marijuana, Gallup … Record High: More Americans Are Trying Marijuana, Gallup Poll Finds. Retrieved December 9, 2021, from https://www.usnews.com/news/national-news/articles/2021-08-17/record-high-more-americans-are-trying-marijuana-gallup-poll-finds.











 By Hannah P.
By Hannah P.