Overview

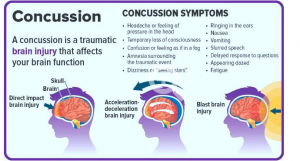
The NFL is among the most watched sports league in the United States, it is also among the leading sports in diagnosed concussions. In 2019, the NFL had 224 diagnosed concussions over their 17-week season (Battista et al 2020). The NFL has been working to implement changes in the game and equipment to help decrease the number of head injuries each year.
Improvements in evaluation
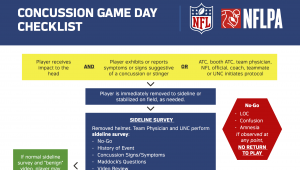
The improvements in the protocol made since 2018 include, defining impact seizure and fencing responses as independent signs of potential loss of consciousness, representing “No-Go” criteria, requiring an evaluation for all players demonstrating gross motor instability to determine the cause of the instability, and requiring all players who undergo any concussion evaluation on game day to have a follow-up evaluation conducted the following day by a member of the medical staff (NFL players health and safety et al., 2021).
Rule changes
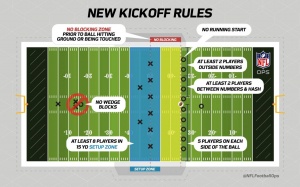
Since 2019, the NFL has implemented 3 new rules to help reduce the number of concussions. The blindside block is eliminated, expanding protection of defenseless players. It is now prohibited for a blocker to initiate forcible contact with his head, shoulder or forearm when his path is toward or parallel to his own end line. This is more of a technique change since concussions tend to be a bigger issue in the inexperienced NFL players. Another rule change was it is now a foul for running forward and leaping across the line of scrimmage in an obvious attempt to block a field goal. This just means you cannot get a running start in order to block a kick which results in less impact. Their last change wasn’t as much of a change, but they decided to keep the kickoff changes made in 2018 as there was a 35% decrease in concussions on kickoffs as a result (NFL Football Operations et al., 2021).
Equipment changes
The NFL uses Radio Frequency Identification (RFID) tags inside of the equipment which detects impact. These RFID tags help the league to collect more information than ever before about the duration and direction of head impacts players experience based on their positions, both during practices and games. The NFL then breaks down the concussion causing impacts and collects information on the players position, acceleration, and forces. This data has helped the NFL develop position specific helmets to help reduce the number of concussions suffered (NFL et al., 2021).
Conclusion
The NFL is continuing to collect impact data, implement new rules, and creating new equipment standards to help reduce the number of concussions each season. The goal of the NFL is to ultimately eliminate concussions from football; there is still a long way to go.
Works cited
Battista, J. (2020, January 23). NFL reveals 2019 Injury Data, hopeful rule changes are working. NFL.com. Retrieved November 14, 2021, from https://www.nfl.com/news/nfl-reveals-2019-injury-data-hopeful-rule-changes-are-working-0ap3000001098679.
Health & Safety Rules Changes. NFL Football Operations. (2021, August). Retrieved from https://operations.nfl.com/the-rules/rules-changes/health-safety-rules-changes/.
NFL. (2021, August 20). Concussion protocol & return-to-participation protocol: Overview. NFL.com. Retrieved from https://www.nfl.com/playerhealthandsafety/health-and-wellness/player-care/concussion-protocol-return-to-participation-protocol.
Nfl. (2021, October 14). Built by data: NFL Helmet Innovation. NFL.com. Retrieved from https://www.nfl.com/playerhealthandsafety/equipment-and-innovation/engineering-technology/built-by-data-nfl-helmet-innovation.





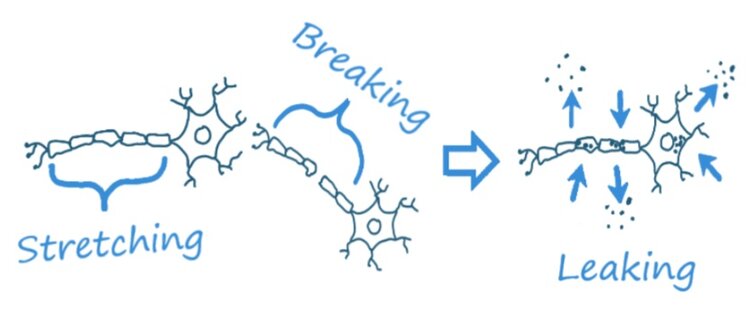 Ionic flux
Ionic flux  becomes “leaky”: notice imag
becomes “leaky”: notice imag