What’s the big idea with tangles?
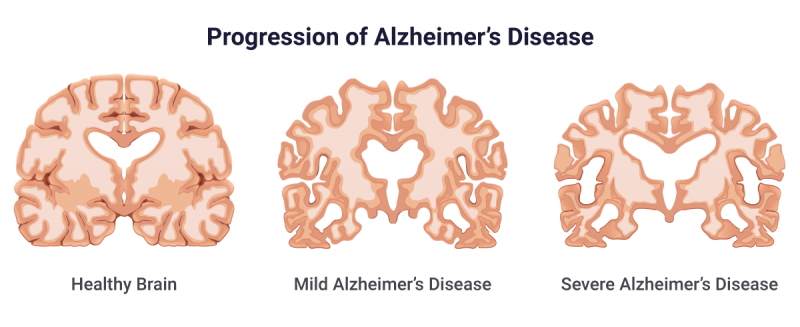
As some of you already know or have heard me talk about, neurofibrillary tangles (NFTs) are insoluble collections of microtubule particles that collect on the inside of a cell in Alzheimer’s disease (AD) patients. These collections of particles occur when the tau protein is hyperphosphorylated and causes it to be misfolded. The tau protein is usually used to help stabilize the structure of microtubules but in this misfolded state, it causes the destruction of these microtubules. This is what cause NFTs!
New to the light in tangles
RBBP7
Knowing how NFTs occur is old news in terms of neurological disorders. So, what have been people been working on since? Well, researchers at ASU-Banner Neurodegenerative Disease Center at the Biodesign Institute have found a correlation between these NFTs and a protein called RBBP7. The dysregulation of this protein appears to be correlated to the eventual development of NFTs.
RBBP7 is exclusively found in Homo Sapiens and is a core histone-binding subunit that may target chromatin remodeling factors to their histone substrates in a way that is regulated by nucleosomal DNA.
The figure above is a picture of RBBP7 coming from the Protein Data Bank (PDB). Because RBBP7 is a part of many complexes that regulate chromatin metabolism, its overexpression has been linked to AD as well as some types of cancers.
MMSE Scores and cognitive decline
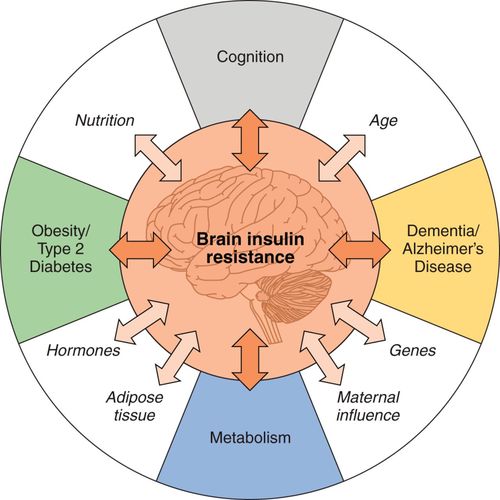
A recent study focused on the combination of NFTs with the amyloid plaques found in AD patients. Most early research involving Alzheimer’s was focused on the amyloid plaques because of the increased toxicity of neurons that they cause. However, it wasn’t until recently that researches have been considering NFTs and amyloid plaques together in the onset of AD.

Figure 1: Pictured above is an example of what an MMSE test is. This test is used to assess the level of cognitive impairment of a patient with a mental disorder. This test is commonly used with AD patients as it can be used to assess the rate at which the patient’s cognitive function is deteriorating.
The research used MMSE scoring to assess how quickly patients with just amyloid plaque build ups decrease from month to month and then compared it to how quickly patients with both amyloid plaques and NFTs decrease from month to month. The study showed that there is a significant increase in degeneration of AD patient’s MMSE scores if both amyloid plaques and tangles are present: amyloid(+)tangle(+) = 0.40 points per month and amyloid(+)tangles(-) = 0.031 points per month.
RNA treatment paves the way to new AD treatments
Another study from August 2021 offers some promising news with NFTs! Research from Boston University School of Medicine discovered:
as the injured nerve cells accumulate misfolded tau protein, they put a tag on RNA, which is the genetic material that codes for proteins. The amount of tagged RNA called N6-Methyladenosine (m6A) increases about four-fold over the course of disease
The research goes on to talk about how inhibiting this RNA-tagging pathway, you can effectively stop neurodegeneration as a result of these tangles. While this research doesn’t address amyloid plaques, this discovery coupled with the one previously stated could mean an effective treatment method to decrease the rate at which neurodegeneration occurs. Sounds pretty promising!



 Eating a healthy diet
Eating a healthy diet