Joy, fulfillment, hope, gratitude, and passion. These are the emotions that come to mind as I reflect on my capstone neurochemistry class and on my Concordia College education as a whole. My four years have been marked by cycles of awe, inquiry, and growth in which my personal and scholarly development far exceeded my expectations. I am deeply grateful for the faculty and peers at Concordia who have shared their wisdom and expertise with me.
This final blog post is rather bittersweet. I’ve anticipated Neurochemistry 475 since my first year because it combines twin passions of mine: a fascination for cellular/molecular neuroscience and a passion for discussion-based humanities courses. I’m struck by how much I already miss this class, especially the community of aspiring neuroscientists (and neuro-interested doctors/dentists/et. al.) who came together with shared goals of understanding more about the brain than we did four months ago.
Reflections on Concordia’s goals for Liberal Learning:
1) Instill a love for learning
My Concordia College education extended my initial love of learning to just about every discipline I’ve encountered on campus, deepening my fierce desire to learn. Neurochemistry followed suit with other upper-division science courses in that concepts I previously thought straightforward turned out to be significantly more complex. Memorable examples include learning that the primary inhibitory neurotransmitter, GABA, actually is excitatory early in development (which blew my mind) and that oxytocin, which I thought was the “love hormone” actually can increase with negative emotional feelings as well. These examples illustrate the enormous complexity of the human brain— after 3.5 years of intensive study, my biggest takeaway is that I really don’t know much at all about how the brain works.
2) Develop foundational skills and transferable intellectual capacities
I’ve expanded my neurochemistry knowledge this semester, and I’ve learned a lot about becoming a scientist, and what sort of scientist I aspire to be. I’ve become much more competent at reading and summarizing primary literature, and at finding and piecing together neurochemical pathways. I’ve developed a foundational knowledge of key signaling pathways (GPCR, RTK, Jak/Stat, and Wnt/β-catenin) which are already useful in other classes and will continue to inform future scholarly work. While these signaling pathways are intrinsically interesting, the best class days were when, like during the addiction unit, we as a class tied intricate neurobiology to real-world examples nearly everyone can relate to.
3) Develop an understanding of disciplinary, interdisciplinary, and intercultural perspectives and their connections
Neurochemistry 475 is a culmination of the neuroscience major, my 7th consecutive chemistry course, my love affair with the nexus of ambitious science and contemplative humanities, and the experience of co-learning with a cohort of highly motivated, compassionate, intelligent students. This class would have been much less impactful if not for the insightful perspectives and knowledge offered by classmates, making our Friday afternoon discussions, whether on Olin Hill, Spread out on the Knutson couches, or virtually via Zoom, so meaningful.
4) Cultivate an examined cultural, ethical, physical, and spiritual self-understanding
I distinctly remember our Friday afternoon discussion on Alzheimer’s Disease—our conversation wrestled with complex philosophical and societal questions about what it means to be a part of the natural aging process, and how best to ameliorate distress in those suffering from dementia/AD. This conversation in particular stands out because of how everyone brought their unique skills and perspectives to the conversation, and I walked away with a richer appreciation for the utter complexity and mystery of neuroscience and broader society. Neurochemistry 475 enabled me to build off of the discussion skills developed throughout my religion, philosophy, and other humanities courses to think through interpersonal/societal consequences of whatever the topic of the week, be it ASD or obesity.
5) Encourage responsible participation in the world
Drawing connections between the sciences and humanities, whether in class, through discussions, or in my blog posts strengthened my desire to continue pursuing science communication throughout my career. Further, the blogs and community action project gave me experience translating relatively high-level neurochemistry concepts to become understandable and interesting for general audiences, a unique and impactful opportunity. This is how I want to do neuroscience, zooming in to understand the molecular mechanisms at play in a given system/disease/ etc., but then zooming out to connect with broader audiences.
Neurochemistry 475 was a key part of my Concordia education, and one I will miss next semester and beyond. Neurochemistry has sharpened my drive to pursue neuroscience, through research, teaching, and outreach, as my vocation and equipped me with technical and conceptual tools to achieve those goals. I’m deeply grateful for Dr. Mach and my classmates who made this class a wonderful learning experience. Thank you.












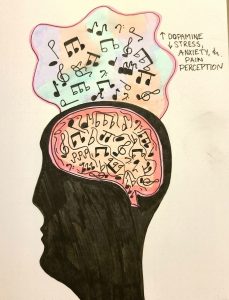


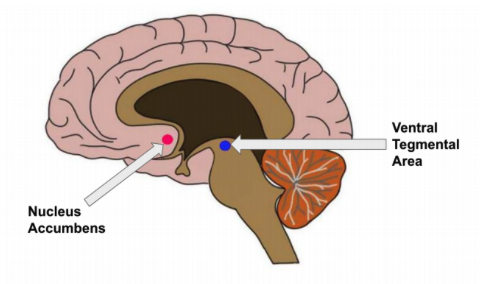 that medication such as opioids do. This in part is why music has been shown to be capable of triggering short-term behavioral changes while also temporarily inhibiting feelings such as stress and/or anxiety. In fact, music that is non-lyrical with a low pitch and/or slow tempo (types that I personal enjoy listening to while studying) have been shown to be most effective at reducing stress and anxiety!
that medication such as opioids do. This in part is why music has been shown to be capable of triggering short-term behavioral changes while also temporarily inhibiting feelings such as stress and/or anxiety. In fact, music that is non-lyrical with a low pitch and/or slow tempo (types that I personal enjoy listening to while studying) have been shown to be most effective at reducing stress and anxiety!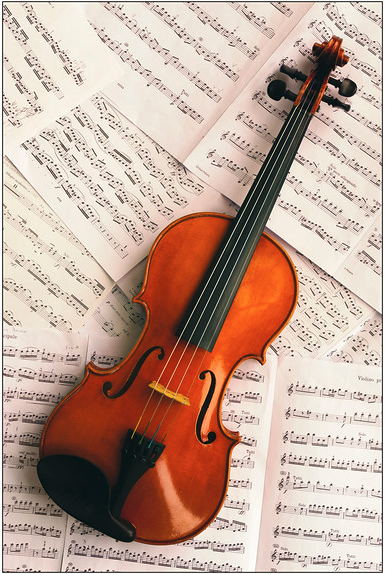 Of course, there will be a select number of individuals who have more benefits through listening, but this is what covers the majority of individuals. There are two factors that this largely comes down to. The first being that playing an instrument is normally far more of an active process than is listening to music. Your fingers and hands are usually both doing different things at the same time while your eyes dart across the sheet music. Most of the time when music is on, the only “active” thing we do is sing along and that can be thought of as more of a pleasurable aspect versus “testing” your brain to see how accurate you can be on wording and pitch. Researchers have been quoted as saying how this process “
Of course, there will be a select number of individuals who have more benefits through listening, but this is what covers the majority of individuals. There are two factors that this largely comes down to. The first being that playing an instrument is normally far more of an active process than is listening to music. Your fingers and hands are usually both doing different things at the same time while your eyes dart across the sheet music. Most of the time when music is on, the only “active” thing we do is sing along and that can be thought of as more of a pleasurable aspect versus “testing” your brain to see how accurate you can be on wording and pitch. Researchers have been quoted as saying how this process “

