In America, it seems that athletics is just as stressed, if not more than, as academics. We live in a culture where professional athletes are praised and put in the spotlight, and the pressure put on them to perform no matter the circumstances is extremely high. So, despite dangerous injuries, professional athletes would often stay in the game to prove their “toughness,” and that tended to be the expectation from coaches since the inception of athletic events. Unfortunately, high school athletes who would follow professional athletes would take cue from them and buy into the idea that they should play at all costs. For specific injuries like concussions, which we now know are extremely dangerous and serious, one important question to ask is why do many high school athletes not report the symptoms of concussion?
Just a Few Reasons
- Winning at all costs
High school athletics are important and are most often extremely beneficial to kids with regards to social connections, teaching discipline, and learning vital teamwork skills. However, far too often are high school athletics not kept in perspective.
 When asked in a study that was published by the Journal of Athletic Training, up to 55% of high school athletes reported that they didn’t or wouldn’t report a concussion. A strong argument could be made that one contributing factor is the athletes did not want to sacrifice playing time to protect their physical health. They are taken too seriously, specifically when it comes to athletes’ injuries.
When asked in a study that was published by the Journal of Athletic Training, up to 55% of high school athletes reported that they didn’t or wouldn’t report a concussion. A strong argument could be made that one contributing factor is the athletes did not want to sacrifice playing time to protect their physical health. They are taken too seriously, specifically when it comes to athletes’ injuries.
2. “I can’t let my team or coach down”
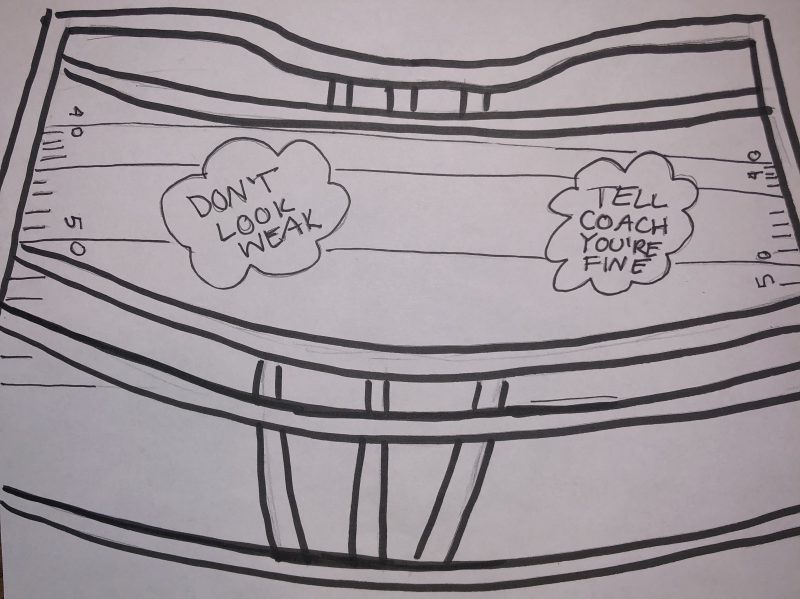
Although a noble motivation, putting the team or opinion of the coach ahead of one’s physical health is extremely risky. Many athletes feel myriad emotions when it comes to physical injuries, and a common one is that they believe they will look “weak” if they complain of pain. According to an article by Reuters Health, males especially tend to be more sensitive to how their fellow teammates and coaches view them. This is arguably due to the expectation that men are supposed to be strong and resilient, and showing emotion is can be considered a “vulnerability” in the sports realm.
3. Honest Ignorance
At higher levels of athletics like college and professional sports, the signs and symptoms of concussions are well known and monitored at the slightest instance of a hit to the head.
However, in high school athletics, strict regulations like that of college and professional sports are not uniformly enforced. This leads to high numbers of ill-informed or uninformed high school athletes and coaching staffs. Not knowing the symptoms of a concussion is dangerous, and too many kids have stated that they did not know they had a concussion while they were concussed.
The Solutions
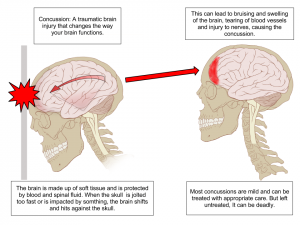
One solution to these problems first and foremost is education. Coaches need to understand the seriousness of concussions and the lasting effects they can have, like difficulty concentrating, personality changes, difficulty with memory, and many more. These are exacerbated if and when someone sustains a second concussion, which is easier to obtain having had an initial concussion. Another point of importance to be stressed to high school athletes, parents of athletes, and coaching staffs is: keep athletics in perspective. Sacrificing enduring brain health problems for a game is never the answer. Brain injuries are unlike injuries to other parts of the body, and injuries to the brain must be treated accordingly. Not to diminish the importance and amazing accomplishments to be had in high school athletics, but after all, it is just a game.
The Science
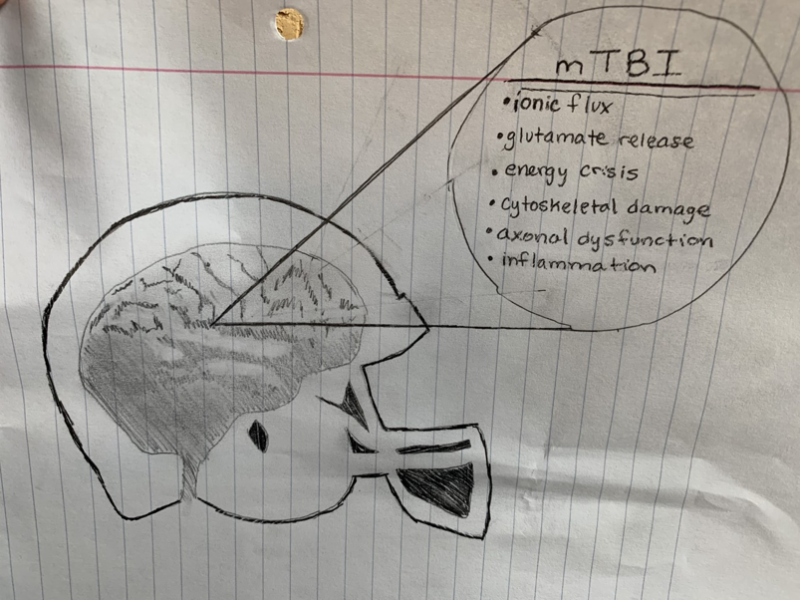
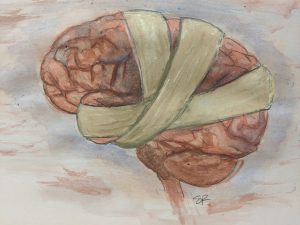
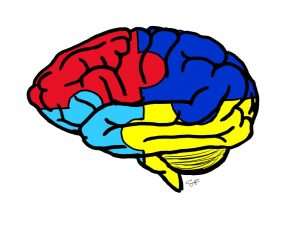
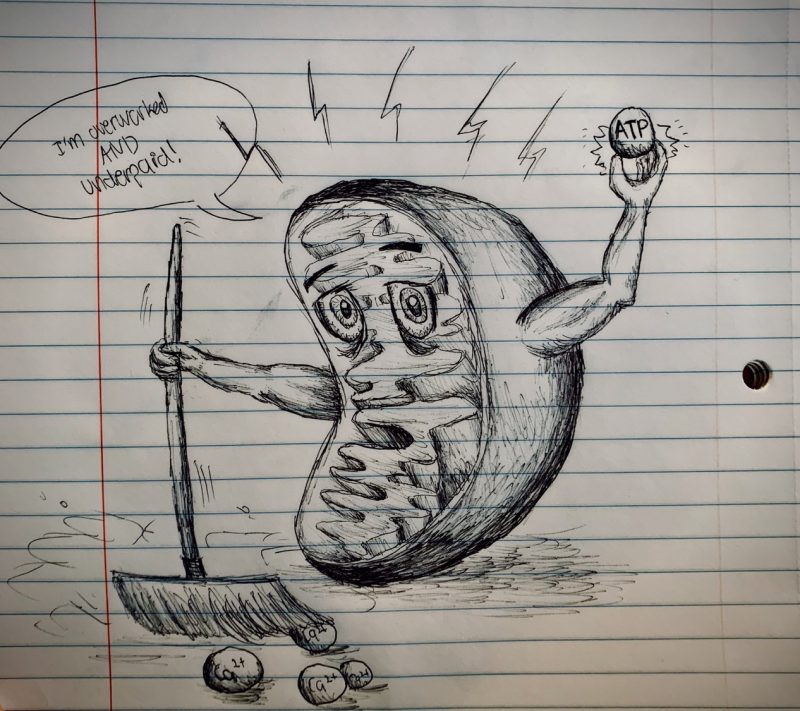
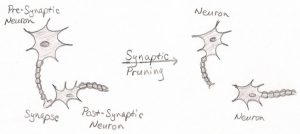
Many things have been studied that occur after a significant impact to the head is sustained. After impact, potassium flows out of the cell while sodium and calcium flows into the cell, and this is allowed because of defects in lipid membranes that occur after the trauma. This causes an ion flux and a subsequent depolarization that can lead to depression-like responses that are attributed to the post-concussive impairments. To combat this, ionic pumps that require ATP are overactive, which leads to hyperglycolysis. This results in an imbalanced energy supply and demand, which ultimately leads to a variety of metabolic changes that are serious to say the least. The force of an impact can also damage the cytoskeletal structures like dendritic arbors, axons, and astrocytic processes. This often leads to the loss of integrity of axons, and in extreme cases axonal disconnection occurs. Overall, it is not just one specific thing that can be pinpointed when determining the cause for a concussion but rather many things that can and do contribute to the effects of a concussion.


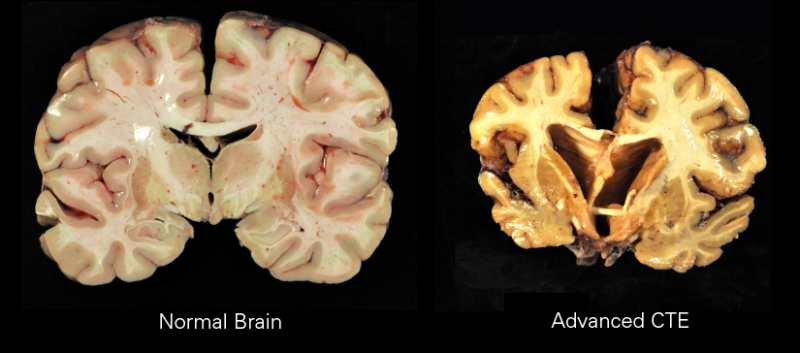



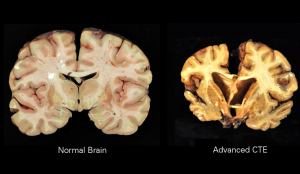


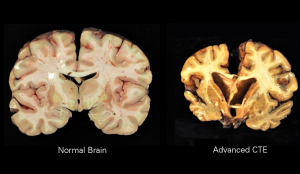 Traumatic Encephalopathy (CTE)
Traumatic Encephalopathy (CTE)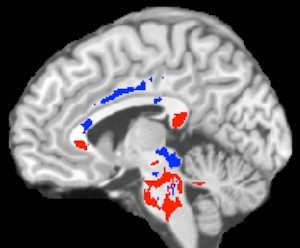 ly rely on neurological and cognitive testing. A neurological test involves tests of vision, hearing, and balance for any deficits that may have been caused by brain trauma. Cognitive tests typically involve tests of memory and concentration that are typically impaired by a concussion.
ly rely on neurological and cognitive testing. A neurological test involves tests of vision, hearing, and balance for any deficits that may have been caused by brain trauma. Cognitive tests typically involve tests of memory and concentration that are typically impaired by a concussion. 
 bly.com/
bly.com/