
Autism is a very broad topic, mostly because the disorder manifests itself differently in every single person who has it. There are people with autism spectrum disorder who have difficulty completing daily tasks. There are also people with the disorder where it is completely invisible. Focusing on the broad, overview of autism masks the more complicated mechanism of the disorder. It is in these mechanisms that treatments for autism and its symptoms lie.
Some Context
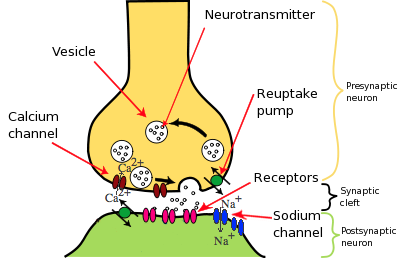
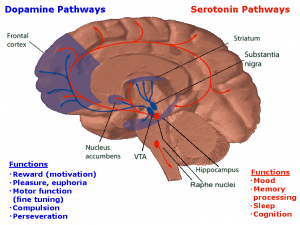
Most neurological disorders can be classified into two categories: too much excitation of the neurons (neurons firing too much) or too much inhibition (neurons not firing enough). For example, excessive excitation in the amygdala is linked to anxiety disorders. Autism arguably fits into both categories, as it is linked to mutations that mess with the balance of inhibitory and excitatory neurons.
How a Cell becomes a Neuron
Our experiences is what drives neuronal development. Excitatory synapses form on the dendritic spines (the spikey parts of the neuron). This makes since as glutamate (an excitatory neurotransmitter) binds to NMDA and AMPA receptors, which promote the development of dendritic spines. Additionally, these receptors help strength the synapse so it fires more quickly.
In our DNA[ii]
We tend to think of DNA as something that is static, like something that is kept up in a safe and rarely pulled out. In reality, DNA is dynamic, playing a vital role in cell functioning and differentiation. How DNA interacts with the rest of the cell is determined by our experiences. For example, glutamate and the NMDA receptors trigger an increase in calcium inside the cell. This activates multiple pathways (outlined in the figure below). These pathways then activate transcription factors, which influence which genes get turned into mRNA. mRNA then helps make the proteins, which perform a specific function.

Autism is a genetic disorder. In the context of transcription, this means that mutated genes get transcribed, altering synaptic growth and development as a result of experience. Well, there are many different genetic mutations that lead to autism, there are two main proteins that are affected: neuroligins and neurexins and SHANK proteins.
Neuroligins and Neurexins
Neuroligins and neurexins are examples of adhesion proteins. They are involved in neuronal differentiation. Neuroligins are post-synaptic proteins, serving as receptors for neurexins. Certain neuroligins are excitatory whilst some are inhibitory. Neurexins help bind other postsynaptic proteins together.
Mice with a mutation on the neuroligin-3 gene show altered social behavior similar to that of autism and increased inhibitory transmission. However, the mice show no problems with excitatory transmission, creating an imbalance between these two types of neurons. Similarly, mice with an overexpression of the Nlgn1 gene (which codes for these proteins) increases excitatory synapses. Overexpression of the normal gene leads to a decrease in excitatory synapses, along with weaken of those present. When the gene is completely removed, problems with NMDA receptor mediated currents arise.
Overall, neuroligins and neurexins affect multiple pathways. All these problems may explain the broadness and diversity among autism.
SHANK
SHANK is a scaffolding protein. (For an explanation of scaffolding proteins, click here). These proteins help in the differentiation and function of synapses. Autism is linked to mutations in three different variants of the SHANK protein, creatively named SHANK1, SHANK2, and SHANK3. Mice without these proteins show varying symptoms. For example, mice without SHANK2 show problems with motor behavior and vocalization whereas those without SHANK3 show more problems with social interaction. All this might explain the diversity of symptoms of autism.[iv]
Comorbidity with Other Disorders
Autism may not be an isolated disorder. In some cases it can be, but it can also be a symptom of larger more complex disorders. Like autism these disorders come from genetic mutations and imbalance in excitatory and inhibitory neurons.
Fragile X syndrome: This disorder is caused by a mutation on the FMRI gene, located on the X chromosome. The mutation leads to a decreased amount of the FMRP protein. This protein plays a vital role in synaptic plasticity, basically ensuring that the synapses stay strong. Without the protein, dendritic spine growth becomes excessive, leading to too many immature spines. This causes behavioral issues and developmental delays.
Tuberous sclerosis complex: This disorder manifests as benign tumors on various organs and often coexists with autism. It is caused by a mutation on two genes that make two proteins: TSC1 and TSC2, both proteins work very closely with brain derived neurotropic factor (BDNF). The exact schematic is described in the figure below. Basically, when the TSC proteins are activated, the activity of GTPase activating protein (GAP) is reduced. This activates the protein Rheb, which in turn activates the protein mTOR. Without the activation of TSC, this pathway is disrupted and abnormal protein synthesis. It is still unclear exactly how this disorder is connected to autism.

Timothy syndrome: This disorder causes complications in many areas of the body. Symptoms include: heart problems, deformities in fingers and toes, problems in the central and peripheral nervous system. It is caused by a mutation in the CACNA1c gene, leading to an increase in calcium ions in the synapse. This leads to activation of a variety of calcium dependent pathways, which are heavily involved in synaptic plasticity and cell growth.
Angelman Syndrome: Typically diagnosed early in life, Angelman syndrome is linked to seizures, lack of coordination, a microcephaly and other symptoms. Unlike other disorders, Angelman syndrome is caused by a deletion of a single allele, chromosomal region 15q11-q13 to be exact. This leads to a loss of UBE3A, a gene that is essential for neuronal growth.
Rett Syndrome: Caused by mutations in the MECP2 gene, Rett syndrome causes motor system disabilities and seizures in addition to autism. Normally, MECP2 is involved in ensuring that DNA is folded into chromatins properly. In Rett syndrome, this is not the case. Additionally, the gene may play a role in regulating the balance between inhibitory and excitatory synapses.
The Forest
Autism is a complicated disorder, with so many varying symptoms and causes. But, this is where hope lies. If improved treatments for autism are going to be developed, this is where they will be. Examining these details can improve the quality of live for people with autism. At the very least, it can help those without empathize with those who have autism.
[i] https://ibguides.com/biology/notes/nerves-and-hormones/
[ii]Image courtesy of pixabay
[iv] Activity-dependent neuronal signaling and autism spectrum disorder
Artstract by Mitzi Probst


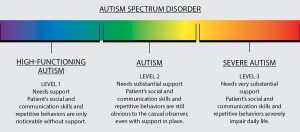


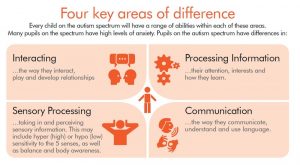
 Autism spectrum disorder (ASD) is a debilitating development disorder. Frequent signs include impairments in social interactions and communication, and restricted, repetitive and stereotyped behaviors or interests. Autism is typically diagnosed in ages 2-3 but can sometimes be diagnosed later in life, especially in females. ASD is primarily a genetic disorder but can also be due to mutations. Some of these are:
Autism spectrum disorder (ASD) is a debilitating development disorder. Frequent signs include impairments in social interactions and communication, and restricted, repetitive and stereotyped behaviors or interests. Autism is typically diagnosed in ages 2-3 but can sometimes be diagnosed later in life, especially in females. ASD is primarily a genetic disorder but can also be due to mutations. Some of these are: and what is happening deep down. Autism is something that one is born with, but is not diagnosed until certain developmental bench marks are missed. Autism is diagnosed and then a spectrum is used to help define the severity. Some who are high functioning are considered to have Asperger’s. Autism is a complex disease and affects each person differently. However, even though they have a disease, they are still people living their life.
and what is happening deep down. Autism is something that one is born with, but is not diagnosed until certain developmental bench marks are missed. Autism is diagnosed and then a spectrum is used to help define the severity. Some who are high functioning are considered to have Asperger’s. Autism is a complex disease and affects each person differently. However, even though they have a disease, they are still people living their life.



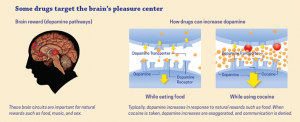
 factor causes more proteins to be produced than normal and affects the neural connections within the brain. Now, understanding slightly better what happens deep in the brain. So, is addiction within a person’s control?
factor causes more proteins to be produced than normal and affects the neural connections within the brain. Now, understanding slightly better what happens deep in the brain. So, is addiction within a person’s control?




 [5]
[5]