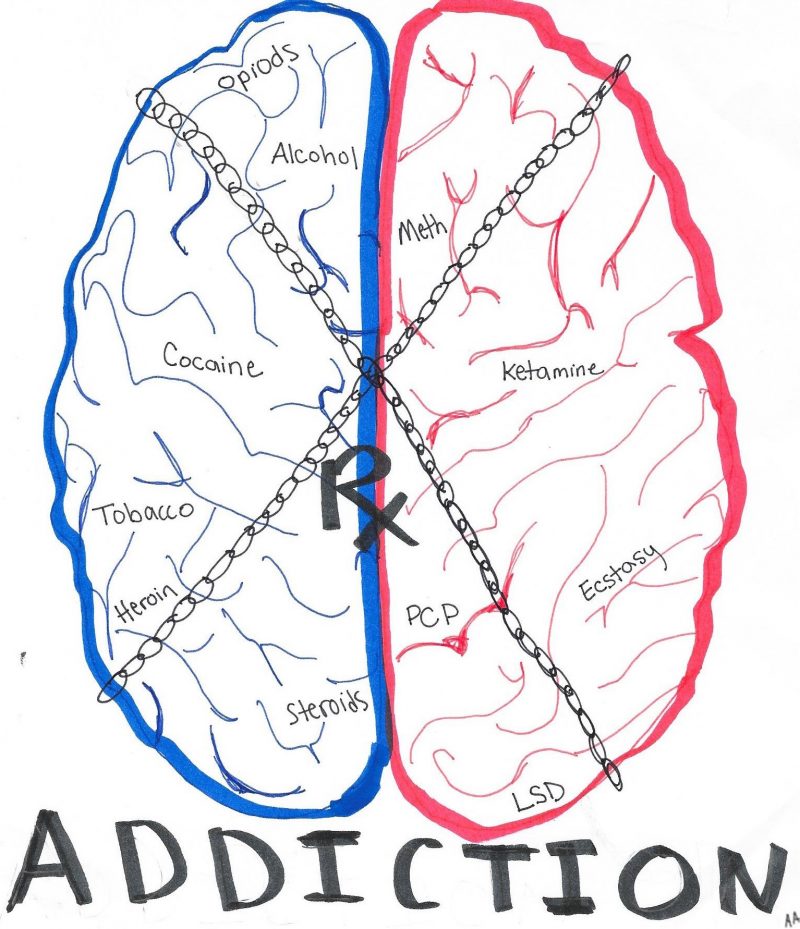
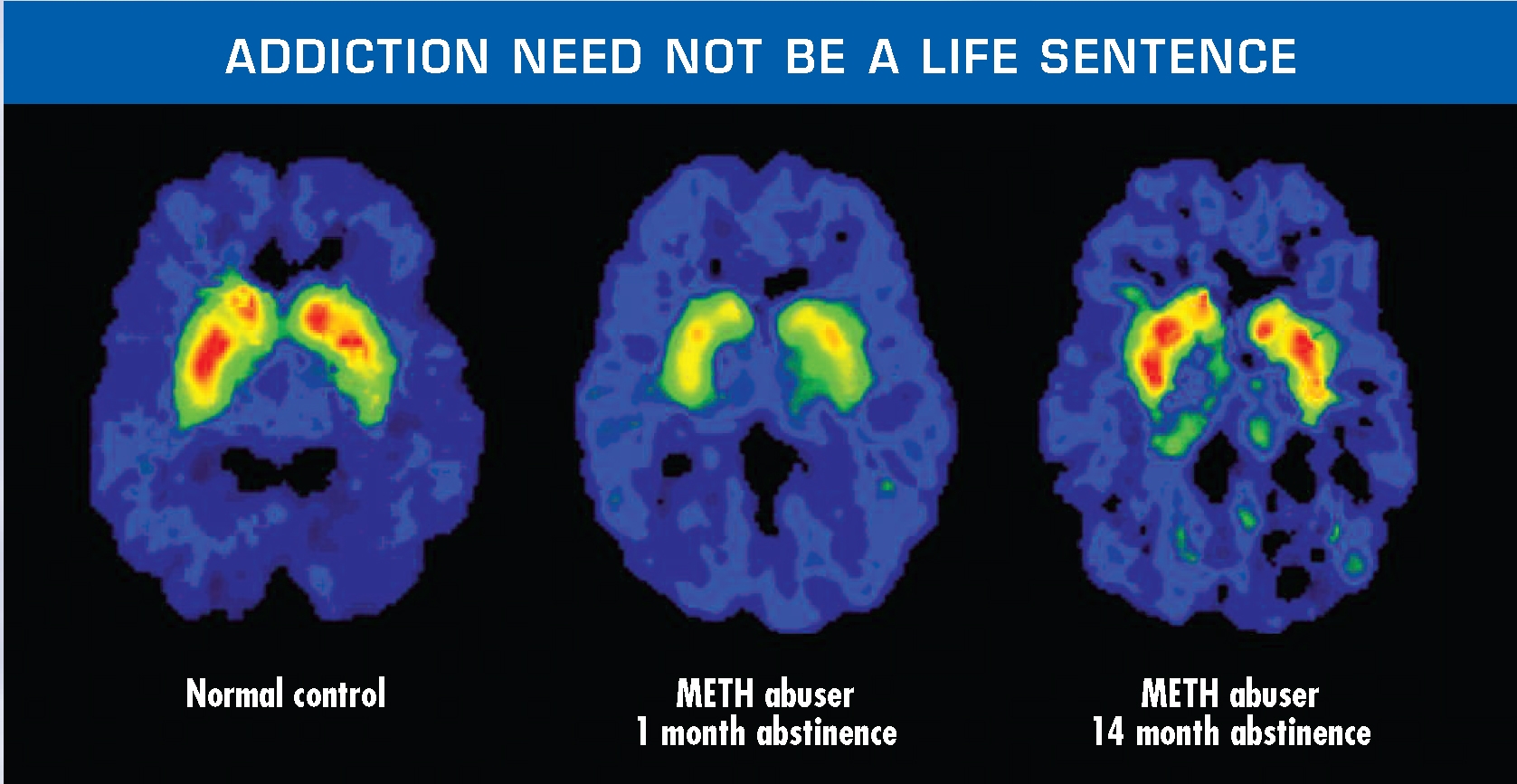
The debate about whether addiction is a disease or an active choice made by the individual has been around for centuries and has largely been an opinion based argument. However, in the past several decades, extensive research has been done to better understand the addiction. The research shows that the sustained use of drugs can alter synapse and lead to chemical imbalances of various neurotransmitters. Research has also shown that addiction shares several physiological pathways with other degenerative disease. This mounting evidence can be used, and rightly should be used to show that addiction is not a choice but rather a complex neurological disease. Classifying addiction as a disease will allow people struggling with the disorder to seek help without fear of ridicule.
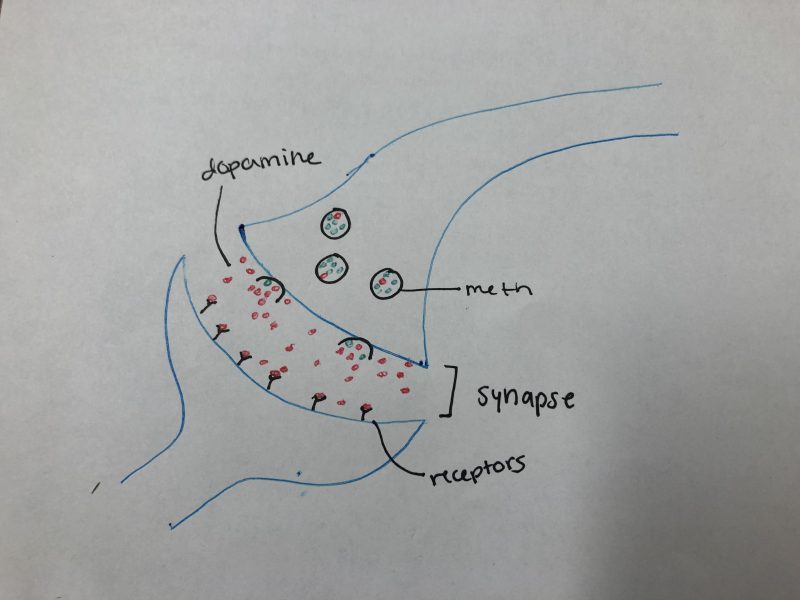
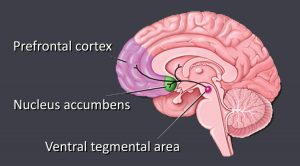
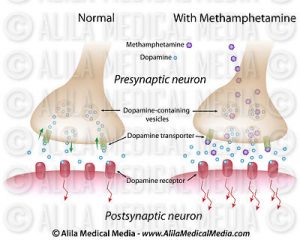
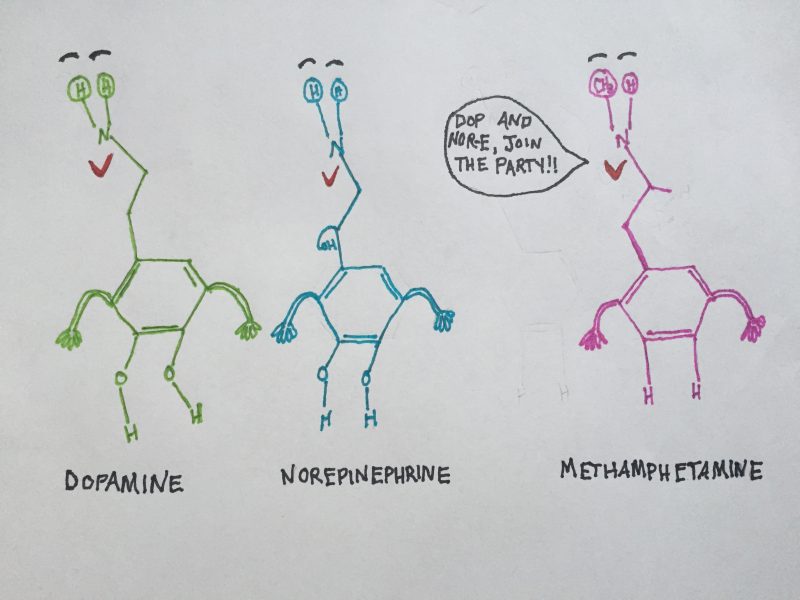
Many drugs affect individuals in similar ways, the difference occurs in how symptoms. Drugs such as cocaine and amphetamines increase levels of dopamine within the neuron. This excess dopamine, which is the main neurotransmitter associated with pleasure binds with D1 receptors in the neuron which increase cAMP. The increase of cAMP increases the activation of PKA and transcription factors such as CREB and delta FOS-B. These transcription factors, then transcribe specific segments of DNA which produces a multitude of proteins. The over activation of these proteins leads to changes in synapse and thus affects neural connections within the brain.
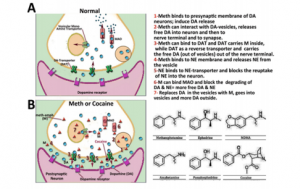
Ok so enough of the nerd talk. Addiction promotes a feel good response in the brain. The chemical that is responsible for this feeling has the ability to change how the brain is “wired” leading to dependence on the drug. More simply put taking drugs change connections in the brain hard wiring users to take and crave the drug.
With the realization that those people addicted to drugs are no longer in control, where does a person put the blame. If an individual is hardwired for a drug, can they really be held responsible for doing things in order to obtain that drug? I’m not attempting to sway individuals one way or another, and honestly, I do not know when blame can be can be shifted from the user to the disease of addiction. Perhaps this depends in some part on the potency of the drug. Different drugs have different potentials thus allowing individuals to become addicted at different rates. Even the issue of initially taking the drug can become very convoluted upon further contemplation. Examining the various social and socioeconomic factors of drug addicts provides several similarities such as poverty, lack of education, violence, and potential even culture. These factors could be used to make the argument that individuals in these circumstances do not have a choice in the initial decision to take the drugs.
The issue of drug abuse and addiction is complicated from a variety of standpoints. The evidence that addiction is in fact a disease is strong. The mechanisms and pathways that various drugs affect synapse connections and neruochemical balances varies, however the feel good chemical dopamine seems to play a major role. The social factors surrounding addiction must also be considered when attempting to assign blame. Can blame be placed on a person who is designed for the drug? How prevalent are the social circumstances of the drug addict? Where does the blame go??
Sources
https://moodle.cord.edu/pluginfile.php/818256/mod_resource/content/0/Overview%20of%20addiction%202019.pdf





 Medications, which are typically antipsychotics, are far from perfect, or even decent; the side effects are horrendous and can be permanent, many medications don’t work well or only treat certain symptoms, and constant dose adjustments must be made to maximize efficiency while limiting negative effects. Due to these problems, many patients with schizophrenia refuse to stay on their medications, raising difficult questions for family members and physicians. Check out this
Medications, which are typically antipsychotics, are far from perfect, or even decent; the side effects are horrendous and can be permanent, many medications don’t work well or only treat certain symptoms, and constant dose adjustments must be made to maximize efficiency while limiting negative effects. Due to these problems, many patients with schizophrenia refuse to stay on their medications, raising difficult questions for family members and physicians. Check out this