“Neurochemistry. What a beautiful word. Chemistry of the brain. It sounds so complex and I’m sure it is.” This is what I thought when I saw this class when I was registering last spring. I really had no idea about what was going on in the brain, I’ve never taken another neuro class so I was really excited to learn about it. I was pleasantly surprised to find out that I had a few great friends that were taking the class as well. I was even more pleasantly surprised to find out that so many of the people in this class that I did not know before have now grown to be my friends. All of this along with learning something new? I couldn’t be happier.
I really enjoyed the community action project that we did with the social work students. So many times in our articles we look at cold, hard, scientific facts that we can use to help treat ailments that come out of some brain problem. However, the social work students remind us to view these people as a whole person, not just a patient in need of our help. This helped to show me that we have to do what is best for the person, not just treat them for the sake of treating them.
My favorite part of neurochemistry was our Friday discussions. Every Friday, we would go sit in some comfortable chairs and discuss what we had learned during the week about our paper. I loved this so much because I got to see so many different perspectives on the same idea. I got to see how somebody would treat a disease as a social issue and how we could possibly solve some of these issues. It gives everyone a good chance to voice some opinions, observations, or shed new light on something that others haven’t thought of before.

https://twitter.com/kernelcobb/status/76844603683661313
Concordia College has Five Goals for Liberal Learning:
- Instill a love for learning
Neurochemistry helped to instill a love for learning in our whole class. Every week there were so many things that were not understood about the paper, so we would take time to ask these questions, look for the answers, and share them with the class.
- Develop foundational skills and transferable intellectual capacities
For me, I found this class to help me work on my critical thinking skills; especially in exams when we were given a problem and we had to deduce how the pathway works and what was going wrong. Regardless of where we will be in our lives in the future, we will likely be working in some type of team. Doing the community action project, doing group discussions, and working together on papers will all help us in the future.
- Develop an understanding of disciplinary, interdisciplinary, and intercultural perspectives and their connections
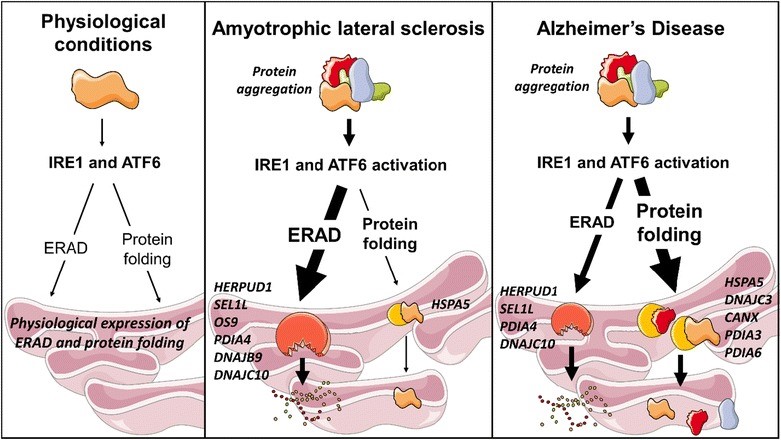
This course helped me to understand different brain disease and how they pervade societally and culturally in our world. We learned about Autism, Alzheimer’s, Anxiety, Schizophrenia, Addiction, Endocannabinoids, ALS, and obesity. All of these are prevalent in our world today and we are trying to connect them back to the brain. If we can better understand these things, we can better treat or fix these problems.
- Cultivate an examined cultural, ethical, physical, and spiritual self-understanding
The thing that gave me the best self-understanding throughout this class was writing these blogs. It really made me think about how I felt with the issue, what I think should be done, and what I still do not really understand. It’s really important to reflect upon your studies to think about these things. Though these blogs may have been “required”, I found myself looking forward to writing them because then I could think back upon the week and about what I learned.
- Encourage responsible participation in the world.
Together with all of the above, I believe that this class has encouraged me to BREW along with many other classes that I have taken in my time here at Concordia College.
So now after reflecting on my time in Neurochemistry I can definitively say that not only is Neurochemistry a beautiful word that is a complex and difficult problem, it is also more important in our world than I could have ever known because of all of its connections and my favorite class that I took at Concordia. I look forward to seeing what my classmates do in their futures and I hope that they all remember this class the same I will. I’m going to remember it as the time that “The Gang Does Neurochemistry”.




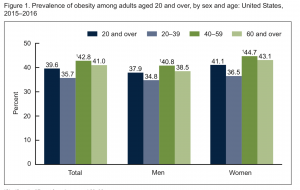
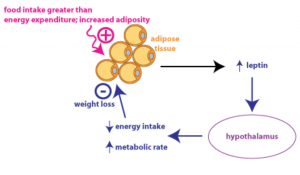
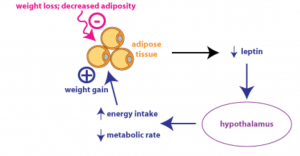
 Obesity is becoming more and more prevalent, as rates climb throughout both adult and youth populations. Around 40% of adults (over 20 years of age) are obese, as well as 20% of children. In the last 15 years alone these rates have shown a great increase. Obesity leads to the development of many serious health issues such as type 2 diabetes, hypertension, steatohepatitis, heart disease, stroke, cancer, depression, sleep apnea… the list goes on and on. To many people who are not obese, it seems as if there should be an easy fix to the obesity epidemic sweeping the nation: eat healthy and exercise. But what if I told you it is not as simple as that? What if I said that obesity can actually be classified as a neurological disorder? Because sometimes, there isn’t a simple answer to losing weight and keeping it off.
Obesity is becoming more and more prevalent, as rates climb throughout both adult and youth populations. Around 40% of adults (over 20 years of age) are obese, as well as 20% of children. In the last 15 years alone these rates have shown a great increase. Obesity leads to the development of many serious health issues such as type 2 diabetes, hypertension, steatohepatitis, heart disease, stroke, cancer, depression, sleep apnea… the list goes on and on. To many people who are not obese, it seems as if there should be an easy fix to the obesity epidemic sweeping the nation: eat healthy and exercise. But what if I told you it is not as simple as that? What if I said that obesity can actually be classified as a neurological disorder? Because sometimes, there isn’t a simple answer to losing weight and keeping it off.
 knowledge to succeed or understand the content in this class. Once we got into the rhythm of the class, I was pleasantly surprised that I was not as behind as I thought. Neurochemistry was a great class to have a capstone experience for many reasons.
knowledge to succeed or understand the content in this class. Once we got into the rhythm of the class, I was pleasantly surprised that I was not as behind as I thought. Neurochemistry was a great class to have a capstone experience for many reasons.