One of the greatest blessings we often take for granted is our privilege to be able-minded and able-bodied. We live our lives boldly, making life goals and holding expectations that often rely on our current functionality. The reality is that one moment can change everything.

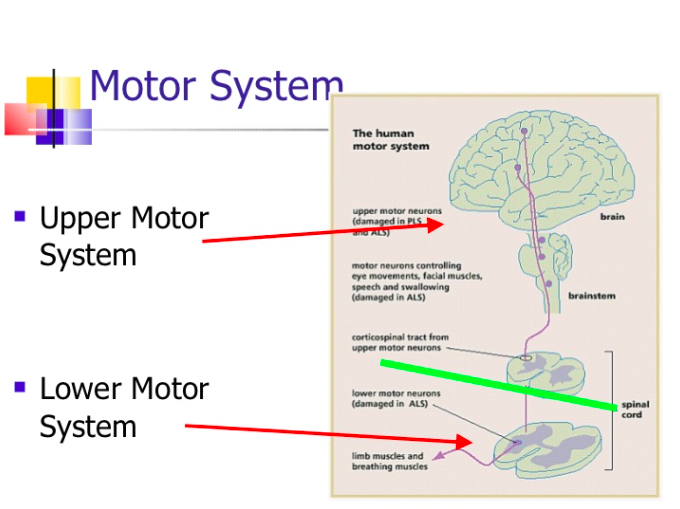
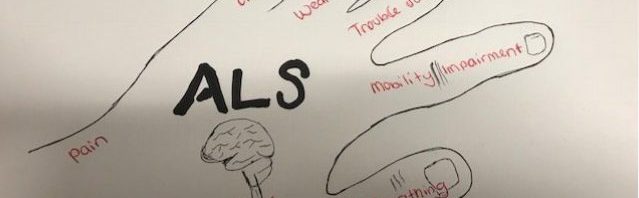
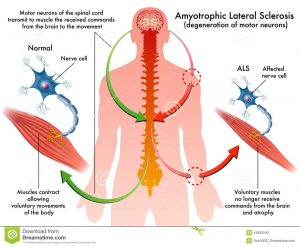
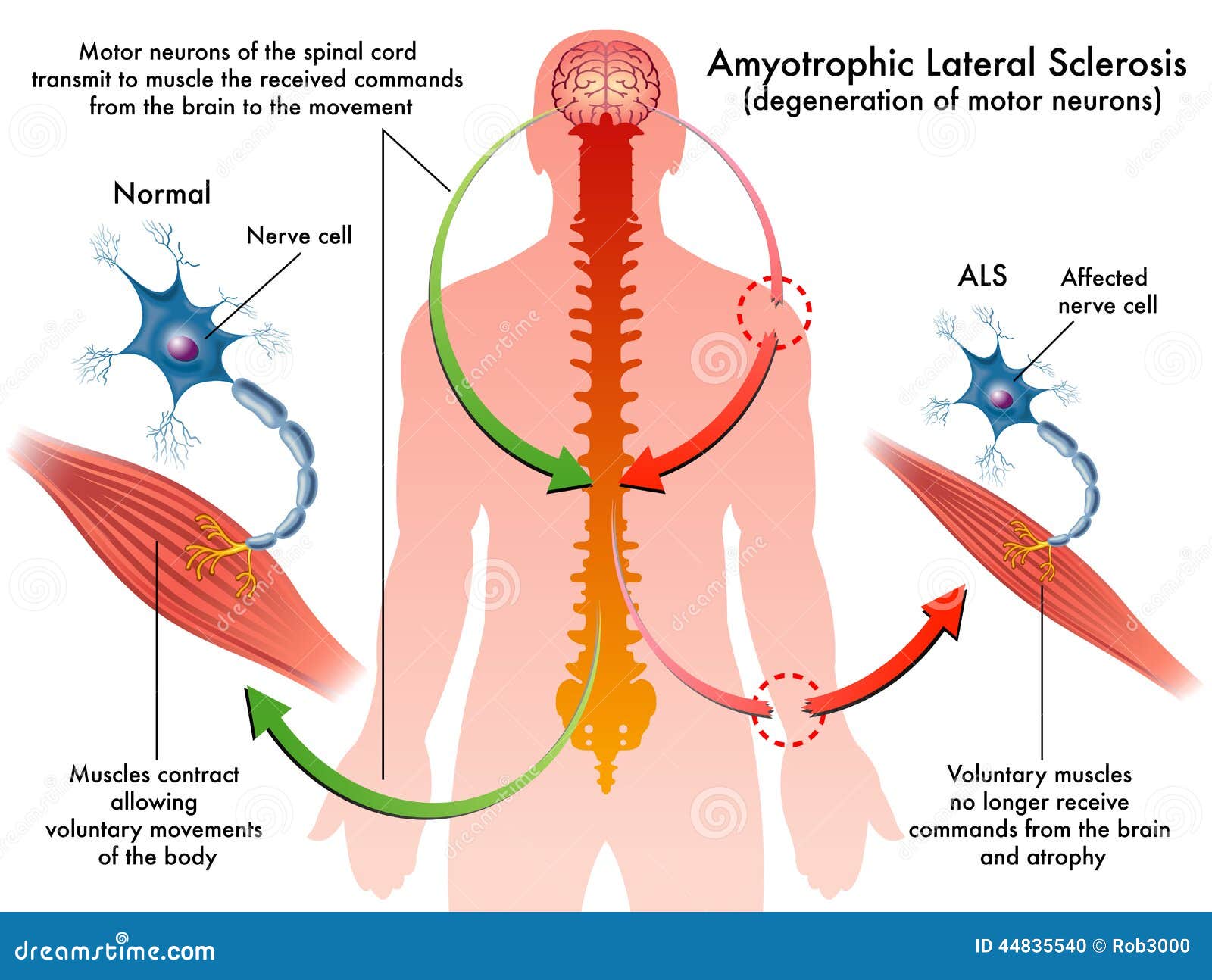
Unfortunately for some, that moment is their diagnosis with a motor neuron disease known as amyotrophic lateral sclerosis (ALS). This disease attacks motor neurons that control your muscle movement, which can progressively affect your ability to run, walk, stand, talk, and eventually breathe.
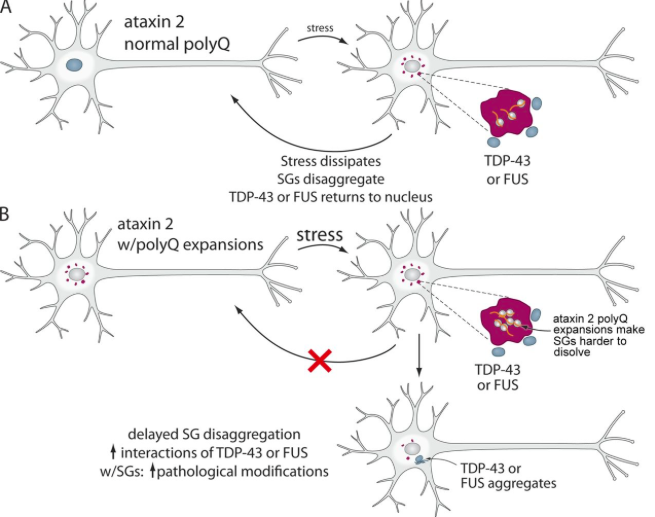
At a neurochemical level, genetic mutations have caused changes in RNA and the mitochondria. As of now, researchers know that oxidative stress is damaging mitochondria and causing RNA dysfunction, as RNA-binding proteins (FUS and TDP43) are being spliced and aggregated within the cytoplasm.
However, this RNA dysfunction is also contributing to the oxidative stress damaging mitochondria. FUS and TDP43 are reducing protection against oxidative stress and upregulating the enzymes responsible for increasing the levels of oxidative stress.
These mutated proteins contribute to misfolded proteins, leading to defective organelles and cell death. Aside from RNA mutations, researchers have also considered the role of iron and copper metabolism and their role in reducing oxidative stress.
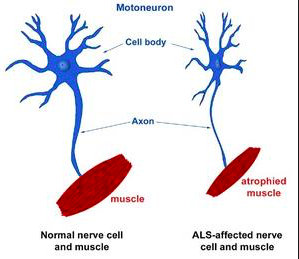
As FUS and TDP43 are accumulating, the motor neuron axons begin to retract because the transporter proteins are not efficiently carrying information down the axon to trigger muscle contraction. As these neurons become less able to communicate their information, the cells become smaller and sometimes die. This cell death is what leads to the muscle atrophy and paralysis commonly associated with ALS.

An ALS diagnosis may bring a feeling of hopelessness. Without previous knowledge or signs of its onset until it has fully progressed, one can feel trapped within their own body. Currently, there is no cure; only treatment to slow its progression. As a society, we need to support those individuals by funneling money toward research to understand the progression of this disease. With these answers, we can seek better treatment and restore hope for those affected by ALS.
Steven Hawking, one of the most insightful intellectuals of our time, expands on his freedom to be able-minded, even though his ALS stripped him of being able-bodied. While most would rightfully feel the burden of the motor neuron disease, Steven’s slow-progressing form of the disease has given him time to reflect on the freedom of being able-minded.

He has proven through his contributions to science and philosophy that life satisfaction is based on perspective: one can feel trapped by the disease, or to use that life-changing diagnosis to redirect their path with the time they have left. I will leave you with my favorite quote of Steven’s:
“There should be no boundaries to human endeavor. We are all different. However bad life may seem there is always something you can do, and succeed at. While there is life, there is hope.”