The perception of marijuana as a “serious drug” has dwindled over the recent decades due to increasing legalization and the portrayal of the drug in the media. As of the end of 2018, marijuana is available for medical purposes in 32 states and the District of Columbia. Although still limited, more research is being conducted on the drug to learn more of its effects on our brain and overall health. However, the process for being able to research the drug is quite intensive; several regulatory barriers block the availability of marijuana. These include going through the following federal agencies:
- National Institute on Drug Abuse (NIDA)
- S. Food and Drug Administration (FDA)
- Drug Enforcement Administration (DEA)
- Other review boards and departments in state government
These roadblocks are due to cannabis’ classification as a Schedule I drug, which was instilled in 1970 in the Controlled Substances Act.
Marijuana and Pain
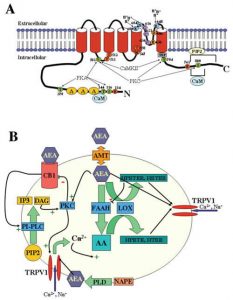
It is widely accepted that marijuana helps treat pain. However, few in the general public know how this happens in the body. In our brains, pain signals are transduced through receptors known as transient receptor potential cation channel receptors (TRPVRs). These receptors are ion channels, and when bound by a ligand (such as capsaicin, an ingredient in hot peppers), they will allow the influx of calcium and sodium to depolarize the cell. This depolarization will allow an action potential of the neuron to transmit the pain signal on. In cannabis, there are compounds known as endocannabinoids (eBCs). These eBCs act as a ligand to the TRPV receptors and cannabinoid (CB) receptors. CB and TRPV receptors are inversely related; when one receptor type is active, the other type is inactive. It is by this mechanism two methods of treating pain are possible:
- CB1 and CB2 receptors bind eCBs (agonists), causing TRPV channel activity to decrease, meaning less pain propagation. CB1 activation decreases neuronal excitability, meaning eCBs can have an anti-inflammatory effect on the brain.
- eCBs, like anandamine, is an agonist for TRPV1, but not as strong of a ligand for the receptor, so there is a reduced signal level for pain. With a constant level of eCBs, the TRPV receptors will also become “desensitized,” resulting in an even weaker signal over time. This mechanism is very helpful for chronic pain.
Using Marijuana to treat addiction and epilepsy
Cannabis not only treats pain, but can also be used as an aid for addiction and preventing seizures in epileptic people. With cannabis having no legal dose, it can used as a replacement of other drugs to rehab from. It has the potential, not yet proven though, to wean an addict off of their drug of abuse. Several studies have been conducted, showing epileptics are seizure-free after just weeks of proper dosing of cannabidiol (CBD) oil. CBD also has the allure of not having the psychoactive part of marijuana THC. With CBD being legal in all 50 states, it can be used for medical purposes all across the nation, and should be researched even more.
Sources:
http://www.governing.com/gov-data/safety-justice/state-marijuana-laws-map-medical-recreational.html
